The main vital function of the respiratory system is to provide tissues with oxygen and remove carbon dioxide.
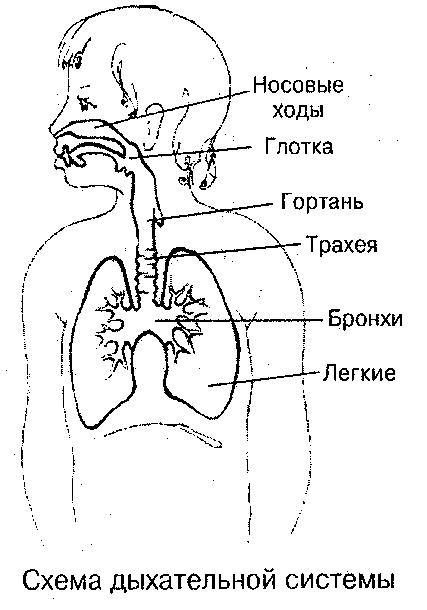
Respiratory organs consist of air-conducting (respiratory) tracts and paired respiratory organs - lungs. The airways are divided into upper (from the opening of the nose to the vocal cords) and lower (larynx, trachea, lobar and segmental bronchi, including intrapulmonary branches of the bronchi). By the time the child is born, their morphological structure is still imperfect, with which the functional characteristics of respiration are also associated.
Intensive growth and differentiation of the respiratory organs continues during the first months and years of life. The formation of the respiratory organs ends on average by the age of 7 and later only their sizes increase.
Anatomical and physiological features. All airways in a child are significantly smaller and narrower than in an adult.
The features of their morphological structure in children of the first years of life are as follows:
1) thin, delicate, easily injured dry mucous membrane with insufficient development of glands, reduced production of secretory immunoglobulin A (SIg A) and surfactant deficiency;
2) rich vascularization under the mucous layer, represented mainly by loose fiber and containing few elastic and connective tissue elements;
3) the softness and compliance of the cartilaginous framework of the lower respiratory tract, the absence of elastic tissue in them and the lungs.
This reduces the barrier function of the mucous membrane, facilitates easier penetration of the infectious agent into the bloodstream, and also creates the prerequisites for narrowing the airways due to the rapidly emerging edema or compression of the compliant respiratory tubes from the outside (thymus gland, abnormally located vessels, enlarged tracheobronchial lymph nodes).
Nose and nasopharyngeal space. In children early age the nose and nasopharyngeal space are small, the nasal cavity is low and narrow due to insufficient development of the facial skeleton. The shells are thick, the nasal passages are narrow, the lower one is formed only by the age of 4. Even slight hyperemia and swelling of the mucous membrane with a runny nose make the nasal passages impassable, cause shortness of breath, and make it difficult to suck on the breast. Cavernous tissue develops by the age of 8-9, therefore, nosebleeds in young children are rare and caused by pathological conditions. They are more common during puberty.
Paranasal (paranasal) sinuses. By the time a child is born, only the maxillary (maxillary) sinuses are formed; the frontal and ethmoid are unclosed protrusions of the mucous membrane, taking shape in the form of cavities only after 2 years, the main sinus is absent. Completely all paranasal sinuses develop by the age of 12-15, but sinusitis can develop in children of the first two years of life.
Nasolacrimal duct. Short, its valves are underdeveloped, the outlet is located close to the corner of the eyelids, which facilitates the spread of infection from the nose to the conjunctival sac.
Pharynx.
In young children, the pharynx is relatively wide, the palatine tonsils are clearly visible at birth, but do not protrude due to the well-developed arches. Their crypts and blood vessels are poorly developed, which to some extent explains the rare diseases of angina in the first year of life. By the end of the first year, the lymphoid tissue of the tonsils, including the nasopharyngeal (adenoids), is often hyperplastic, especially in children with diathesis. Their barrier function at this age is low, like in lymph nodes. The overgrown lymphoid tissue is colonized by viruses and microorganisms, foci of infection are formed - adenoiditis and chronic tonsillitis. At the same time, frequent tonsillitis, acute respiratory viral infections are noted, nasal breathing is often disturbed, the facial skeleton changes and an "adenoid face" is formed.
Epiglottis.
Closely related to the root of the tongue. In newborns, it is relatively short and wide. The incorrect position and softness of its cartilage can cause functional narrowing of the entrance to the larynx and the appearance of noisy (stridor) breathing.
Larynx. In children, the larynx is higher than in adults, it drops with age, and is very mobile. Its position is unstable, even in the same patient. It has a funnel-shaped shape with a distinct narrowing in the region of the subglottic space, bounded by the rigid cricoid cartilage. The diameter of the larynx in this place in a newborn is only 4 mm and increases slowly (6-7 mm at 5-7 years, 1 cm by 14 years), its expansion is impossible. A narrow lumen, an abundance of nerve receptors in the subglottic space, easily occurring edema of the submucosal layer can cause severe breathing disorders even with small manifestations respiratory infection (croup syndrome).
Thyroid cartilage in young children forms an obtuse rounded corner, which becomes more acute in boys after 3 years. From the age of 10, a characteristic male larynx is already formed. True vocal cords in children are shorter than in adults, which explains the pitch and timbre of a child's voice.
Trachea.
In children of the first months of life, the trachea is often funnel-shaped; at an older age, cylindrical and conical shapes predominate. Its upper end is located in newborns much higher than in adults (at the level of IV and VI cervical vertebrae, respectively), and gradually descends, like the level of tracheal bifurcation (from the III thoracic vertebra in a newborn to V-VI at 12-14 years old). The frame of the trachea consists of 14-16 cartilaginous half-rings, connected behind by a fibrous membrane (instead of an elastic end plate in adults). The membrane contains many muscle fibers, the contraction or relaxation of which changes the lumen of the organ.
The child's trachea is very mobile, which, along with the changing lumen and softness of the cartilage, sometimes leads to its slit-like collapse on exhalation (collapse) and is the cause of expiratory shortness of breath or rough snoring breathing (congenital stridor). Stridor symptoms usually disappear by age 2 when the cartilage becomes denser.
Bronchial tree.
By the time of birth, the bronchial tree is formed. As the child grows, the number of branches and their distribution in the lung tissue do not change. The size of the bronchi increases intensively in the first year of life and in puberty. They are also based on cartilaginous half rings, which do not have a closing elastic plate in early childhood, connected by a fibrous membrane containing muscle fibers. The cartilage of the bronchi is very elastic, soft, springy and easily displaced. The right main bronchus is usually an almost direct continuation of the trachea, therefore it is in it that foreign bodies.
The bronchi, like the trachea, are lined with multi-row columnar epithelium, the ciliated apparatus of which is formed after the birth of the child. Hyperemia and edema of the bronchial mucosa, its inflammatory swelling significantly narrow the lumen of the bronchi, up to their complete obstruction. So, with an increase in the thickness of the mucous layer and mucous membrane by 1 mm, the total area of \u200b\u200bthe lumen of the bronchi of a newborn decreases by 75% (in an adult - by 19%). The active motility of the bronchi is insufficient due to the weak development of muscles and ciliated epithelium.
Incomplete myelination of the vagus nerve and underdevelopment of the respiratory muscles contribute to the weakness of the cough impulse in a small child; Infected mucus accumulating in the bronchial tree clogs the lumens of the small bronchi, contributes to atelectasis and infection of the lung tissue. Thus, the main functional feature of the bronchial tree of a small child is the insufficient performance of the drainage, cleansing function.
Lungs.
In a child, as in adults, the lungs have a segmental structure. The segments are separated from each other by narrow grooves and interlayers of connective tissue (lobular lung). The main structural unit is the acinus, but its terminal bronchioles end not in a bunch of alveoli, as in an adult, but in a sac (sacculus). From the "lace" edges of the latter, new alveoli are gradually formed, the number of which in a newborn is 3 times less than in an adult. The diameter of each alveoli also increases (0.05 mm in a newborn, 0.12 mm at 4-5 years old, 0.17 mm at 15 years old). At the same time, the vital capacity of the lungs increases.
The interstitial tissue in the child's lung is loose, rich in blood vessels, fiber, contains very few connective tissue and elastic fibers. In this regard, the lungs of a child in the first years of life are more full-blooded and less airy than that of an adult. Underdevelopment of the elastic frame of the lungs contributes to both the occurrence of emphysema and atelectasis of the lung tissue. Atelectasis especially often occurs in the posterior lower parts of the lungs, where hypoventilation and blood stagnation are constantly observed due to the forced horizontal position of a small child (mainly on the back).
The tendency to atelectasis is enhanced by a deficiency of surfactant, a film that regulates surface alveolar tension and is produced by alveolar macrophages. It is this deficiency that leads to insufficient expansion of the lungs in premature infants after birth (physiological atelectasis), and also underlies the respiratory distress syndrome, which is clinically manifested by severe respiratory failure.
Pleural cavity. The child is easily stretchable due to the weak attachment of the parietal sheets. The visceral pleura, especially in newborns, is relatively thick, loose, folded, contains villi, outgrowths, most pronounced in the sinuses, interlobar grooves. In these areas, there are conditions for a more rapid emergence of infectious foci.
Lung root.
Consists of large bronchi, vessels and lymph nodes (tracheobronchial, bifurcation, bronchopulmonary and around large vessels). Their structure and function are similar to those of peripheral lymph nodes. They easily react to the introduction of infection - a picture of both nonspecific and specific (tuberculous) bronchoadenitis is created. The lung root is an integral part of the mediastinum.
The latter is characterized by slight displacement and is often the site of development of inflammatory foci, from where the infectious process spreads to the bronchi and lungs. A pitchfork gland (thymus) is also placed in the mediastinum, which is large at birth and normally gradually decreases during the first two years of life. An enlarged thymus gland can cause compression of the trachea and large vessels, disrupt breathing and blood circulation.
Diaphragm.
Due to the peculiarities chest the diaphragm plays an important role in the breathing mechanism in a small child, providing depth of inhalation. The weakness of her contractions is partly due to the newborn's extremely shallow breathing. Any processes that impede the movement of the diaphragm (formation of a gas bubble in the stomach, flatulence, intestinal paresis, enlargement of parenchymal organs, intoxication, etc.), reduce ventilation of the lungs (restrictive respiratory failure).
The main functional physiological features of the respiratory system are as follows:
1) the depth of breathing, the absolute and relative volumes of one respiratory act in a child is much less than in an adult. These indicators gradually increase with age. When crying, the volume of respiration increases 2-5 times. The absolute value of the minute volume of respiration is less than that of an adult, and the relative value (per 1 kg of body weight) is much larger;
2) the respiratory rate is higher, the younger the child. It compensates for the small volume of each respiratory act and provides oxygen to the child's body. Rhythm instability and short (3-5 min) respiratory arrests (apnea) in newborns and premature infants are associated with incomplete differentiation of the respiratory center and its hypoxia. Oxygen inhalation usually eliminates respiratory arrhythmias in these children;
3) gas exchange in children is carried out more vigorously than in adults, due to the rich vascularization of the lungs, blood flow rate, high diffusion capacity. At the same time, the function external respiration in a small child it is disturbed very quickly due to insufficient excursions of the lungs and expansion of the alveoli.
Edema of the epithelium of the alveoli or interstitium of the lungs, switching off even a small area of \u200b\u200blung tissue from the act of breathing (atelectasis, stagnation in the posterior lower parts of the lungs, focal pneumonia, restrictive changes) reduce pulmonary ventilation, cause hypoxemia and the accumulation of carbon dioxide in the blood, i.e., the development of respiratory failure, as well as respiratory acidosis. Tissue respiration is carried out in a child at a higher energy expenditure than in adults, and is easily disturbed with the formation of metabolic acidosis due to the instability of enzyme systems inherent in early childhood.
Research methodology.
When assessing the state of the respiratory system, questioning (usually of the mother) and objective methods are used - examination and counting of the number of respiratory movements, palpation, percussion, auscultation, as well as laboratory and instrumental studies.
Inquiry. The mother is asked how the perinatal period and childbirth proceeded, how the child was ill, including shortly before the present disease, what symptoms were observed at the onset of the disease. Pay special attention to nasal discharge and difficulty in nasal breathing, the nature of the cough (periodic, paroxysmal, barking, etc.) and breathing (hoarse, wheezing, audible at a distance, etc.), as well as contacts with patients with respiratory or other acute or chronic infection.
Visual inspection. Examination of the face, neck, chest, extremities gives the more information the younger the child. Pay attention to the cry, voice and cough of the child. The examination helps to identify, first of all, signs of hypoxemia and respiratory failure - cyanosis and shortness of breath.
Cyanosis can be pronounced in some areas (nasolabial triangle, fingers) and be common. With advanced microcirculation disorders, a rough cyanotic (marble) pattern on the skin is observed. Cyanosis can occur with screaming, swaddling, feeding, or persistent.
Expansion of the superficial capillary network in the zone VII of the cervical vertebra (Frank's symptom) may indicate an increase in tracheobronchial lymph nodes. A pronounced vasculature on the skin of the chest is sometimes an additional symptom of hypertension in the pulmonary artery system.
Dyspnea is often accompanied by the involvement of the accessory muscles and retraction of the compliant regions of the chest.
Inspiratory dyspnea with difficult, sonorous, sometimes wheezing inspiration is observed in croup syndrome and any obstruction of the upper airways.
Expiratory dyspnea with difficulty and prolongation of exhalation is characteristic of obstructive bronchitis, bronchial asthma, bronchiolitis, viral respiratory syncytial infection, and a significant increase in tracheobronchial lymph nodes.
Mixed dyspnea is observed with pneumonia, pleurisy, circulatory disorders, restrictive respiratory failure (severe flatulence, ascites). Puffing dyspnea of \u200b\u200ba mixed nature is noted with severe rickets.
Swelling and tightening of the wings of the nose indicates difficulty breathing and is equivalent to shortness of breath in newborns and children in the first months of life.
You should also pay attention to nasal discharge and its nature. Sacral, especially unilateral discharge can be observed with a foreign body in the nasal passages or nasal diphtheria. Pink foam that comes out of the nose and mouth is one of the symptoms of acute pneumonia in newborns.
The child's voice allows you to judge the state of the upper respiratory tract. A hoarse, low-pitched voice or full aphonia is characteristic of laryngitis and croup syndrome. A harsh, low voice is characteristic of hypothyroidism. A nasty, nasal tinge acquires a voice with chronic rhinitis, adenoids, paresis of the palatine curtain (with birth trauma, poliomyelitis, diphtheria), tumors and abscesses of the pharynx, congenital defects in the development of the upper jaw.
The cry of a healthy full-term baby is loud, sonorous, promotes the expansion of lung tissue and the disappearance of atelectasis. A premature and debilitated baby has a weak cry. Crying after feeding, before defecation, during urination requires the elimination of hypo-galaxies, anal fissures, phimosis, vulvitis and urethritis, respectively. A periodic loud cry is often observed with otitis media, meningitis, abdominal pain, monotonous inexpressive "cerebral" cry - with organic damage to the central nervous system.
Coughis a very valuable diagnostic feature. To artificially induce a cough, you can press on the cartilage of the trachea, the root of the tongue, irritate the pharynx. A barking, rough cough that gradually loses its sonority is characteristic of croup syndrome. A paroxysmal, prolonged cough consisting of successive cough shocks, accompanied by a sounding labored inhalation (reprise) and ending with vomiting, is observed with whooping cough.
Bitonal cough is characteristic of enlargement of tracheobronchial and bifurcational intrathoracic lymph nodes. A short, painful cough with a wheezing exhalation often occurs with pleuropneumonia; dry, painful - with pharyngitis, tracheitis, pleurisy; wet - with bronchitis, bronchiolitis. It must be remembered that swelling of the nasopharyngeal mucosa, enlargement of the adenoids, excessive mucus formation can cause persistent cough, especially when changing position and without affecting the underlying airways.
The counting of the number of respiratory movements should be made at the beginning of the examination at rest (or sleep), since the child easily develops tachypnea with any impact, including emotional. Bradi-pnea in children is rare (with meningitis and other brain lesions, uremia). In case of severe intoxication, breathing of the "driven animal" is sometimes observed - frequent and deep. The counting is done within a minute, better in sleeping children and by respiratory noises, through a phonendoscope brought to the nose. In older children, counting is done with a hand placed on the chest and abdomen at the same time (on the costal arch), since children tend to have abdominal or mixed breathing patterns. The respiratory rate of a newborn child is 40-60 per minute, one-year-old - 30-35, 5-6 years old - 20-25.10 years - 1Ya-20, an adult -15-16 per minute.
Palpation.
Palpation reveals chest deformities (congenital, associated with rickets or other bone formation defects). In addition, the thickness of the skin fold is determined symmetrically on both sides of the chest and the swelling or retraction of the intercostal spaces, the lag of one half of the chest during breathing. Edema of tissue, a thicker fold on one side, bulging of the intercostal spaces are characteristic of exudative pleurisy. The retraction of the intercostal spaces can be observed with atelectasis and adhesion processes in the cavity of the pleura and pericardium.
Percussion.
In children, percussion has a number of characteristics:
1) the position of the child's body should ensure the maximum symmetry of both halves of the chest. Therefore, the back is percussed when the child is standing or sitting with legs crossed or outstretched, the lateral surfaces of the chest - in a standing or sitting position with hands on the back of the head or extended forward, and the chest is lying;
2) percussion should be quiet - finger on finger or direct, since the child's chest resonates much more than that of an adult;
3) the finger-plessimeter is located perpendicular to the ribs, which creates conditions for a more uniform formation of percussion tone.
Percussion tone in a healthy child of the first years of life is usually high, clear, with a slightly boxy shade. When screaming, it can change - from a distinct tympanitis on maximum inhalation and shortening on exhalation.
Any stable change in the nature of the percussion tone should alert the doctor. In bronchitis, bronchiolitis, asthmatic syndrome and asthma, and often bronchopneumonia with small foci of pulmonary tissue compaction and vicarious emphysema, a boxy or high-pitched tympanic sound may occur. With pneumonia, especially protracted and chronic, a "motley" sound is possible - alternating sections of tone shortening and percussion tympanic sound. A significant local or total shortening of the tone indicates massive (lobar, segmental) pneumonia or pleurisy. The enlargement of the tracheobronchial lymph nodes is detected with direct percussion along the spinous processes of the vertebrae, starting from the lower thoracic regions.
The shortening of the sound below the II thoracic vertebra indicates a possible bronchoadenitis (a symptom of the Corany de la Campa).
The boundaries of the lungs are determined along the same lines as in adults, on average 1 cm higher due to the higher standing of the diaphragm (in children of early and preschool age). The mobility of the pulmonary margin is determined when the child is breathing freely.
Auscultation. Features of the technique: 1) strictly symmetrical position of both halves of the chest, similar to that of percussion; 2) the use of a special children's stethoscope - with long tubes and a small diameter, since the membrane can distort the sound.
Heard normal breathing sounds depend on age: up to 6 months in a healthy child, weakened vesicular breathing due to its superficial nature; at the age of 6 months - 7 years, puerid (baby) breathing is heard, with a more distinct inhalation and a relatively louder and longer exhalation. In school-age children and adolescents, breathing is the same as in adults - vesicular (the ratio of the duration of inhalation and exhalation is 3: 1). When a child screams, performing auscultation is no less valuable than at rest. When crying, the depth of inhalation increases, bronchophonia is well defined, which intensifies over the areas of compaction of the lung tissue, various wheezing is heard.
Pathological breathing sounds include the following types of breathing:
1) bronchial (the ratio of the duration of inhalation and exhalation 1: 1), observed during infiltration of the lung tissue and above the zone of the lung compressed by fluid or air, while the extended exhalation indicates bronchospasm;
2) weakened vesicular in children over one year old with pleurisy, tuberculous infiltration of lung tissue, painful inhalation (with rib fracture, myositis, appendicitis, peritonitis), severe bronchial obstruction, foreign body;
3) amphoric, heard over bullous (with destructive pneumonia) and other cavities in the lungs.
Wheezing is heard during various pathological processes in the bronchi and lungs, most often at the depth of inspiration. Dry rales of a wired nature (rough, sonorous, whistling) are heard in case of laryngitis, pharyngitis, tracheitis, asthmatic bronchitis, a foreign body, an attack of bronchial asthma. In the latter case, they can be heard from a distance. Wet rales - large and medium bubbly - indicate the defeat of the bronchi; small, voiced are formed in the bronchioles, crepitant - in the alveoli.
The prevalence and stability of hearing wheezing are of diagnostic value: small and crepitant wheezing, locally determined for a long time, rather indicate a pneumonic focus. Diffuse, intermittent, variegated moist rales are more characteristic of bronchitis or bronchiolitis.
For bronchoadenitis, symptom D "Espina" is characteristic - a clear listening to whispering speech over the spinous processes below the thoracic vertebra I. The pleural friction noise is determined in pleurisy and is characterized in children by instability, transient nature.
The oropharynx is examined last in the child. The patient's head and hands are securely fixed by the mother or a nurse, with the help of a spatula, first examine the mucous membrane of the cheeks, gums, teeth, tongue, hard and soft palate. Then, with a spatula, press down on the root of the tongue and examine the palatine tonsils, arches, and the posterior pharyngeal wall. In small children, the epiglottis can often be examined. The main signs of lesions of the oropharynx, which are of diagnostic value, see Digestive and Abdominal Organs.
Laboratory and instrumental research.
The following studies have the greatest diagnostic value:
1) X-ray;
2) bronchological;
3) determination of gas composition, blood pH, acid-base balance;
4) functions of external respiration;
5) analysis of bronchial secretions.
The features of instrumental laboratory research in pediatric practice are as follows:
1) technical difficulties of bronchological research associated with the small size of the airways;
2) the use of general anesthesia, especially in young children, for bronchoscopy and bronchography;
3) compulsory participation in bronchological examination of specialists - pediatrician, pediatric bronchopulmonologist, anesthesiologist;
4) the impossibility of using the most common spirographic determination of the function of external respiration in children under 5-6 years old and the use of pneumography and general plethysmography in this contingent of patients;
5) difficulties in conducting gas analytical studies in newborns and children under 3 years of age due to rapid breathing and a negative attitude towards the methods used.
By the end of the 3rd - at the beginning of the 4th week of embryonic development, a protrusion of the wall of the anterior intestine appears, from which the larynx, trachea, bronchi and lungs are formed. This protrusion grows rapidly, a bulbous expansion appears at the caudal end, which divides into the right and left parts at the 4th week (future right and left lungs). Each part is further divided into smaller branches (future shares). The resulting protrusions grow into the surrounding mesenchyme, continuing to divide and again forming spherical extensions at their ends - the rudiments of the bronchi of ever smaller caliber. In the 6th week, lobar bronchi, on the 8-10th - segmental bronchi. Formation begins from the 16th week respiratory bronchioles. Thus, by the 16th week, the bronchial tree is mainly formed. This is the so-called glandular stage of lung development. From the 16th week, the formation of a lumen in the bronchi begins (recanalization stage), and from the 24th - the formation of future acini (alveolar stage),does not end before birth, the formation of alveoli continues in the postnatal period. By the time of birth, there are about 70 million primary alveoli in the fetal lungs. Formation of the cartilaginous framework of the trachea and bronchi begins from the 10th week, from the 13th week the formation of glands in the bronchi begins, which contribute to the formation of a lumen. Blood vessels are formed from the mesenchyme at the 20th week, and motor neurons - from the 15th week. The vascularization of the lungs occurs especially quickly at 26-28 weeks. Lymphatic vesselsare formed in the 9-10th week, first in the area of \u200b\u200bthe lung root. They are fully formed at birth.
Formation of acini, which began from the 24th week, does not end at birth, and their formation continues in the postnatal period.
By the time the baby is born, the airways (larynx, trachea, bronchi and acini) are filled with fluid, which is a secretion product of the airway cells. It contains a small amount of protein and has a low viscosity, which facilitates its rapid absorption immediately after birth, from the moment respiration is established.
The surfactant, the layer of which (0.1-0.3 microns) covers the alveoli, begins to be synthesized at the end of intrauterine development. Methyl and phosphocholine transferase are involved in the synthesis of the surfactant. Methyltransferase starts to form from 22-24 weeks of intrauterine development, and its activity progressively increases towards birth. Phosphocholine transferase usually matures only by 35 weeks of gestation. A deficiency in the surfactant system underlies the respiratory distress syndrome, which is more common in premature infants, clinically manifesting as severe respiratory failure.
The given information on embryogenesis suggests that congenital stenosis of the trachea and agenesis of the lung are the result of developmental disorders at very early stages of embryogenesis. Congenital lung cysts are also a consequence of bronchial malformation and accumulation of secretions in the alveoli.
The part of the anterior intestine, from which the lungs originate, later turns into the esophagus. If the correct process of embryogenesis is disturbed, a message remains between the primary intestinal tube (esophagus) and the grooved protrusion (trachea) - esophageal-tracheal fistulas.Although this pathological condition in newborns is rare, nevertheless, if it is present, their fate depends on the time of diagnosis and the speed of providing the necessary medical care. A newborn with such a developmental defect in the first hours looks quite normal and breathes freely. However, at the very first attempt at feeding, due to the ingress of milk from the esophagus into the trachea, asphyxia occurs - the child turns blue, a large number of wheezing is heard in the lungs, and the infection quickly joins. Treatment of such a malformation is only operative and should be carried out immediately after the diagnosis is made. A delay in treatment causes severe, sometimes irreversible, organic changes in the lung tissue due to the constant ingress of food and gastric contents into the trachea.
It is customary to distinguish upper (nose, throat), average (larynx, trachea, lobar, segmental bronchi) and lower (bronchioles and alveoli) airways. Knowledge of the structure and function of various parts of the respiratory system is of great importance for understanding the characteristics of the defeat of the respiratory system in children.
Upper respiratory tract.Nose the newborn is relatively small, its cavities are poorly developed, the nasal passages are narrow (up to 1 mm). The lower nasal passage is absent. The cartilage of the nose is very soft. The mucous membrane of the nose is tender, rich in blood and lymphatic vessels... By the age of 4, the lower nasal passage is formed. As the facial bones (upper jaw) grow and teeth erupt, the length and width of the nasal passages increase. In newborns, the cavernous part of the submucous tissue of the nose is underdeveloped, which develops only by 8-9 years. This explains the relative rarity of nosebleeds in children 1 year of age. Due to the insufficient development of the cavernous tissue in young children, the inhaled air is weakly warmed up, in this regard, children cannot be taken outside at temperatures below -10 ° C. A wide nasolacrimal duct with underdeveloped valves promotes the transition of inflammation from the nose to the mucous membrane of the eyes. Due to the narrowness of the nasal passages and the abundant blood supply to the mucous membrane, the appearance of even a slight inflammation of the nasal mucosa causes difficulty in breathing through the nose in young children. Breathing through the mouth in children of the first half of life is almost impossible, since the large tongue pushes the epiglottis backward.
Although the paranasal sinuses begin to form in the prenatal period, they are insufficiently developed at birth (Table 1).
Table 1
Development of the paranasal sinuses (sinuses) of the nose
|
Sinus name |
The term of intrauterine development, mass |
Size to birth, mm |
Fastest development period |
X-ray detection time |
|
Lattice |
By the age of 7-12 | |||
|
Maxillary |
2-7 years old | |||
|
Frontal |
Slowly up to 7 years, fully developed by 15-20 years | |||
|
Wedge-shaped |
Slowly until age 7, fully developed by age 15 |
These features explain the rarity of diseases such as sinusitis, frontal sinusitis, ethmoiditis, polysinusitis (a disease of all sinuses) in early childhood. When breathing through the nose, air passes with greater resistance than when breathing through the mouth, therefore, when breathing through the nose, the work of the respiratory muscles increases and breathing becomes deeper. The atmospheric air passing through the nose is warmed up, humidified and purified. The warming of the air is the greater, the lower the outside temperature. So, for example, the air temperature when passing through the nose at the larynx level is only 2 ... 3 ° C lower than body temperature. In the nose, the inhaled air is purified, and foreign bodies larger than 5-6 microns are captured in the nasal cavity (smaller particles penetrate into the underlying sections). In the nasal cavity, 0.5-1 l of mucus is released per day, which moves in the back 2/3 of the nasal cavity at a speed of 8-10 mm / min, and in the anterior third - 1-2 mm / min. Every 10 minutes, a new layer of mucus passes, which contains bactericidal substances (lysozyme, complement, etc.), secretory immunoglobulin A.
Pharynx the newborn is narrow and small. The lymphopharyngeal ring is poorly developed. Both palatine tonsils in newborns do not normally extend due to the arches of the soft palate into the pharynx cavity. In the second year of life, hyperplasia of the lymphoid tissue is observed, and the tonsils come out from behind the anterior arches. Crypts in the tonsils are poorly developed, therefore, although there are sore throats in children under one year old, they are less common than in older children. By the age of 4-10, the tonsils are already well developed and can easily hypertrophy. Tonsils are similar in structure and function to lymph nodes.
Tonsils are like a filter for microorganisms, but with frequent inflammatory processes, a focus of chronic infection can form in them. At the same time, they gradually increase, hypertrophy - chronic tonsillitis develops, which can occur with general intoxication and cause sensitization of the body.
The nasopharyngeal tonsils can enlarge - these are the so-called adenoid vegetations, which disrupt normal nasal breathing, and, being a significant receptor field, can cause allergies, intoxication of the body, etc. Children with adenoids are inattentive, which affects their studies at school. In addition, the adenoids contribute to the formation of a malocclusion.
Among the lesions of the upper respiratory tract in children, rhinitis and tonsillitis are most often observed.
Middle and lower respiratory tract.Larynx to the birth of a child has a funnel-shaped form, its cartilage is tender and pliable. The glottis is narrow and located high - at the level of the IV cervical vertebra (in adults - at the level of the VII cervical vertebra). The cross-sectional area of \u200b\u200bthe airway under the vocal folds is on average 25 mm, and the length of the vocal folds is 4-4.5 mm. The mucous membrane is tender, rich in blood and lymph vessels. The elastic tissue is poorly developed. Up to 3 years of age, the shape of the larynx is the same in boys and girls. After 3 years, the angle of connection of the thyroid plates in boys sharpens, which becomes especially noticeable by the age of 7; by the age of 10 in boys, the larynx is similar to the larynx of an adult male.
Glottis remains narrow up to 6-7 years. True vocal folds in young children are shorter than in older children (this is why they have a high voice); from the age of 12, the vocal folds in boys become longer than in girls. The peculiarity of the structure of the larynx in young children also explains the frequency of its defeat. (laryngitis), moreover, they are often accompanied by difficulty in breathing - croup.
Trachea almost completely formed by the time the child is born. It has a funnel shape. Its upper edge is located at level IV of the cervical (in an adult at level VII) vertebra. The bifurcation of the trachea lies higher than that of an adult. It can be roughly defined as the intersection of the lines drawn from spinae scapulae to the spine. The mucous membrane of the trachea is tender and rich in blood vessels. The elastic tissue is poorly developed, and its cartilaginous framework is soft and easily narrows the lumen. With age, the trachea increases both in length and in diameter, however, compared with the growth of the body, the rate of increase in the trachea lags behind, and only from the period of puberty, the increase in its size is accelerated.
The diameter of the trachea changes during the respiratory cycle. The lumen of the trachea changes especially significantly during coughing - the longitudinal and transverse dimensions decrease by 1/3. In the mucous membrane of the trachea there are many glands - approximately one gland per 1 mm 2 of the surface. Due to the secretion of the glands, the surface of the trachea is covered with a layer of mucus 5 microns thick, the speed of mucus movement is 10-15 mm / min, which is ensured by the movement of the cilia of the ciliated epithelium (10-35 cilia per 1 micron 2).
The structural features of the trachea in children determine its frequent isolated lesions. (tracheitis), in combination with a lesion of the larynx (laryngotracheitis) or bronchi (tracheobronchitis).
Bronchi by the time of birth they are well formed. The mucous membrane has a rich blood supply, is covered with a thin layer of mucus, which moves at a speed of 0.25-1 cm / min. In the bronchioles, the movement of mucus is slower (0.15-0.3 cm / min). The right bronchus is, as it were, a continuation of the trachea, it is shorter and somewhat wider than the left.
Muscle and elastic fibers in children of the first year of life are still poorly developed. With age, both the length and the lumen of the bronchi increase. The bronchi grow especially rapidly in the first year of life, then their growth slows down. During the onset of puberty, their growth rate increases again. By the age of 12-13, the length of the main bronchi doubles, with age, the resistance to the collapse of the bronchi increases. In children, acute bronchitis is a manifestation of respiratory viral infection... Less commonly, asthmatic bronchitis is observed with respiratory allergies. The tenderness of the structure of the mucous membrane of the bronchi, the narrowness of their lumen also explain the relatively frequent occurrence in young children bronchiolitis with complete or partial obstruction syndrome.
Lung mass at birth is 50-60 g, which is 1/50 of body weight. In the future, it increases rapidly, and especially intensively during the first 2 months of life and during puberty. It doubles by 6 months, triples by a year of life, increases almost 6 times by 4-5 years, 10 times by 12-13 years, and 20 times by 20 years.
In newborns, lung tissue is less airy and is characterized by the abundant development of blood vessels and loose connective tissue in the septa of the acini. The elastic tissue is insufficiently developed, which explains the relatively easy occurrence of emphysema in various pulmonary diseases. So, the ratio of elastin and collagen in the lungs (dry tissue) in children under 8 months is 1: 3.8, while in an adult it is 1: 1.7. By the time the baby is born, the actual respiratory part of the lungs (acinus, where gas exchange between air and blood occurs) is not sufficiently developed.
Alveoli begin to form from the 4th to 6th week of life, and their number increases very rapidly during the first year, growing up to 8 years, after which the increase in lungs occurs due to the linear size of the alveoli.
Accordingly, the increase in the number of alveoli increases the respiratory surface, especially significantly - during the first year.
This corresponds to the greater oxygen demand of children. By birth, the lumen of the terminal bronchioles is less than 0.1 mm, by 2 years it doubles, by 4 it triples and by 18 years it increases 5 times.
The narrowness of the bronchioles explains the frequent occurrence of atelectasis of the lungs in young children. AI Strukov identified 4 periods in the development of the lungs in children.
In period I (from birth to 2 years) there is a particularly intensive development of the alveoli.
In the II period (from 2 to 5 years) elastic tissue, muscle bronchi with peribronchial and lymphoid tissue included in it develop intensively. Probably, this explains the increase in the number of cases of pneumonia with a protracted course and the beginning of the formation of chronic pneumonia in children in preschool age.
ATIII period (5-7 years) the final maturation of the acinus structure occurs, which explains the more benign course of pneumonia atchildren of preschool and school age.
In the IV period (7-12 years) there is an increase in the mass of mature lung tissue.
As you know, the right lung consists of three lobes: upper, middle and lower, and the left - of two: upper and lower. The middle lobe of the right lung corresponds to the lingual lobe in the left lung. The development of individual lobes of the lung is uneven. In children 1 year of life, the upper lobe of the left lung is less developed, and the upper and middle lobes of the right lung have almost the same size. Only by the age of 2 years, the sizes of individual lobes of the lung correspond to each other, as in adults.
Along with dividing the lungs into lobes in recent years, knowledge of the segmental structure of the lungs has become of great importance, since it explains the peculiarities of the localization of lesions and is always taken into account in surgical interventions on the lungs.
As mentioned, the formation of the lung structure occurs depending on the development of the bronchi. After dividing the trachea into right and left bronchi, each of them is divided into lobar, which are suitable for each lobe of the lung. Then the lobar bronchi are divided into segmental. Each segment looks like a cone or pyramid with the apex directed towards the root of the lung.
Anatomical and functional features of the segment are determined by the presence of self-ventilation, terminal artery and intersegmental septa made of elastic connective tissue. The segmental bronchus with the corresponding blood vessels occupies a certain area in the lobe of the lung. The segmental structure of the lungs is well expressed already in newborns. In the right lung, 10 segments are distinguished, in the left lung - 9 (Fig. 1).
Figure: 1. Segmental structure of the lungs
Upper left and right lobes divided into 3 segments: upper apical (1), upper-posterior (2) and upper front (3). Sometimes another additional segment is mentioned - axillary, which is not considered independent.
Middle right lobe divided into 2 segments: interior (4) located medially, and outer (5), located laterally. In the left lungaverage share corresponds reed, also consisting of 2 segments - upper lingual (4) and inferior lingual (5).
The lower lobe of the right lung is divided into 5 segments: basal-apical (6), basal-medial (7), basal-anterior (8), basal-lateral (9) and basal-posterior (10).
The lower lobe of the left lung is divided into 4 segments: basal-apical (6), basal-anterior (8), basal-lateral (9) and basal-posterior (10).
In children, the pneumonic process is most often localized in certain segments, which is associated with the peculiarities of their aeration, the drainage function of their bronchi, the evacuation of secretions from them and the possibility of infection. Most often, pneumonia is localized in the lower lobe, namely in the basal-apical segment (6). This segment is to a certain extent isolated from the other segments of the lower lobe. Its segmental bronchus extends above the other segmental bronchi and goes straight back at a right angle. This creates conditions for poor drainage, since young children are usually in the supine position for a long time. Along with the defeat of the 6th segment, pneumonia is also often localized in the upper-posterior (2) segment of the upper lobe and the basal-posterior (10) segment of the lower lobe. This is what explains the frequent form of the so-called paravertebral pneumonia. A special place is occupied by the defeat of the middle lobe - with this localization, pneumonia is acute. There is even a term "Mid-lobe syndrome".
The mid-lateral (4) and mid-anterior (5) segmental bronchi are located in the region of the bronchopulmonary lymph nodes; they have a relatively narrow lumen, considerable length, and recede at right angles. As a result, the bronchi are easily compressed by enlarged lymph nodes, which suddenly leads to the shutdown of a significant respiratory surface and is the cause of the development of severe respiratory failure.
|
|
The respiratory tract is a whole complex of formations, the most important functions of which are the distribution of air for the exchange of gases, the delivery of oxygen and the removal of carbon dioxide. Respiratory development begins at the 3rd week of embryonic development and continues for a long time after the birth of the child. By the age of 7, the formation of the respiratory organs ends and in the future there is only an increase in their size. The upper respiratory tract includes the nasal cavity, pharynx and larynx, the lower - the trachea and bronchi. Respiratory organs in children are relatively smaller and are characterized by incomplete anatomical and histological development. |
Figure: 4. Diagram of the structure of the respiratory system.
Nose a young child is relatively small, the nasal passages are narrow, the lower nasal passage is absent. The mucous membrane of the nose is tender, relatively dry, rich in blood vessels. Due to the narrowness of the nasal passages and the abundant blood supply to their mucous membranes, even minor inflammation causes difficulty in breathing through the nose in young children. Breathing through the mouth in children of the first six months of life is impossible, since the large tongue pushes the epiglottis backward. Particularly narrow in young children is the exit from the nasal choana, which is often the cause of long-term disturbance of their nasal breathing.
Paranasal sinuses in young children, they are very poorly developed or completely absent. As the facial bones (upper jaw) increase in size and teeth erupt, the length and width of the nasal passages and the volume of the paranasal sinuses increase. By the age of 2, the frontal sinus appears, the maxillary cavity increases in volume. By the age of 4, the lower nasal passage appears. These features explain the rarity of diseases such as sinusitis, frontal sinusitis, ethmoiditis, in early childhood. Due to the insufficient development of the cavernous tissue in young children, the inhaled air is weakly warmed, in this regard, children cannot be taken out into the street at temperatures below -10 ° C. The cavernous tissue develops well by the age of 8-9, this explains the relative rarity of nosebleeds in children 1 year of life. A wide nasolacrimal duct with underdeveloped valves promotes the transition of inflammation from the nose to the mucous membrane of the eyes. Passing through the nose, atmospheric air is warmed, humidified and purified. In the nasal cavity, 0.5 - 1 liter of mucus is released per day. Every 10 minutes, a new layer of mucus passes through the nasopharynx, which contains bactericidal substances (lysozyme, complement, etc.), secretory immunoglobulin A.
Pharynx in children it is relatively narrow and has a more vertical direction than in adults. Lymphopharyngeal ring in newborns it is poorly developed. The pharyngeal tonsils become visible only by the end of the 1st year of life. Therefore, sore throats in children under 1 year old are less common than in older children. By the age of 4 - 10, the tonsils are already well developed, and their hypertrophy can easily occur. In puberty, the tonsils begin to undergo a reverse development. Tonsils are like a filter for microbes, but with frequent inflammatory processes, a focus of chronic infection can form in them, causing general intoxication and sensitization of the body. The proliferation of adenoids (nasopharyngeal tonsil) is most pronounced in children with constitutional abnormalities, in particular with lymphatic-hypoplastic diathesis. With a significant increase in adenoids - 1.5 - 2nd degree - they are removed, since nasal breathing is disturbed in children (children breathe with an open mouth - the air is not cleared and is not warmed up by the nose, and therefore they often get colds), the shape of the face changes (adenoid face), children become absent-minded (mouth breathing distracts attention), their academic performance deteriorates. When breathing through the mouth, posture is also disturbed, adenoids contribute to the formation of an incorrect bite.
Eustachian tubes in young children, they are wide, and when the child is in a horizontal position, the pathological process from the nasopharynx easily spreads to the middle ear, causing the development of otitis media.
Larynx in young children, it has a funnel-shaped shape (later - cylindrical) and is located slightly higher than in adults (at the level of the 4th cervical vertebra in a child and the 6th cervical vertebra in an adult). The larynx is relatively longer and narrower than in adults, its cartilage is very malleable. The false vocal cords and mucous membrane are delicate, rich in blood and lymphatic vessels, and the elastic tissue is poorly developed.
Glottis in children it is narrow. Vocal cordsyoung children are shorter than older children, so they have a high voice. From the age of 12, boys 'vocal cords become longer than girls'. These features of the larynx explain the easy development of stenotic phenomena in children, even with moderate inflammatory changes in the mucous membrane of the larynx. The increased neuromuscular excitability of a small child is also of great importance. The hoarseness of the voice, often noted in young children after screaming, often depends not on inflammation, but on the weakness of the easily fatigued muscles of the vocal cords.
Trachea in newborns, funnel-shaped, its lumen is narrow, back wall has a wider fibrous part, the walls are more pliable, the cartilage is soft, easily compressed. Its mucous membrane is delicate, rich in blood vessels and rather dry due to insufficient development of mucous glands, elastic tissue is poorly developed. The secretion of the glands provides a layer of mucus on the surface of the trachea with a thickness of 5 microns, the speed of which is 10 - 15 mm / min (provided by cilia - 10 - 30 cilia per 1 micron 2). The growth of the trachea occurs in parallel with the growth of the body, most intensively - in the 1st year of life and in puberty. Structural features of the trachea in children lead to an easy occurrence of stenotic phenomena during inflammatory processes, frequent isolated (tracheitis), combined with damage to the larynx (laryngotracheitis) or bronchi (tracheobronchitis), are determined. In addition, due to the mobility of the trachea, its displacement may occur during a one-sided process (exudate, tumor).
Bronchi sufficiently well formed at birth. The growth of the bronchi is intense in the 1st year of life and in puberty. Their mucous membrane is richly vascularized, covered with a layer of mucus, which advances at a speed of 3 - 10 mm / min, in the bronchioles more slowly - 2 - 3 mm / min. The right bronchus is like a continuation of the trachea, it is shorter and wider than the left. This explains the frequent ingress of a foreign body into the right main bronchus. The bronchi are narrow, their cartilage is soft. Muscle and elastic fibers in children of the 1st year of life are not yet sufficiently developed. The tenderness of the mucous membrane of the bronchi, the narrowness of their lumen explain the frequent occurrence of bronchiolitis in young children with the syndrome of complete or partial obstruction.
Lungs newborns weigh about 50 g, by 6 months. their mass doubles, triples by the year, increases 10 times by the age of 12, and 20 times by the age of 20. Pulmonary slits are poorly expressed. In newborns, the lung tissue is less airy, with abundant development of blood vessels and connective tissue in the septa of the acini and insufficient amount of elastic tissue. The latter circumstance explains the relatively easy occurrence of emphysema in various pulmonary diseases. The poor development of elastic tissue is partly due to the tendency of young children to atelectasis, which is also facilitated by insufficient chest excursion, narrowness of the bronchi. This is also facilitated by insufficient surfactant production, primarily in premature babies. Atelectasis is especially easy in the posterior lower parts of the lungs, since these parts are especially poorly ventilated due to the fact that the child lies on his back almost all the time, and blood stagnation easily occurs. Acini are not sufficiently differentiated. In the process of postnatal development, alveolar passages with typical alveoli are formed. Their number increases rapidly within 1 year and continues to grow up to 8 years. This leads to an increase in the respiratory surface. The number of alveoli in newborns (24 million) is 10 to 12 times, and their diameter (0.05 mm) is 3 to 4 times less than in adults (0.2 to 0.25 mm). The amount of blood flowing through the lungs per unit of time is more in children than in adults, which creates the most favorable conditions for gas exchange in them.
The formation of the lung structure occurs depending on the development of the bronchi. After dividing the trachea into right and left main bronchi, each of them is divided into lobar bronchi, which are suitable for each lobe of the lung. Then the lobar bronchi are divided into segmental. Each segment has independent ventilation, an end artery and intersegmental septa made of elastic connective tissue. The segmental structure of the lungs is already well pronounced in newborns. In the right lung, 10 segments are distinguished, in the left - 9. The upper left and right lobes are divided into three segments - 1, 2 and 3, the middle right lobe - into two segments - the 4th and 5th. In the left lung, the middle lobe corresponds to the reed, also consisting of two segments - the 4th and 5th. The lower lobe of the right lung is divided into five segments - 6, 7, 8, 9 and 10th, the left lung - into four segments - 6, 8, 9 and 10th. In children, the pneumonic process is most often localized in certain segments (6, 2, 10, 4, 5), which is associated with the peculiarities of aeration, drainage function of the bronchi, evacuation of secretions from them and possible infection.
External respiration, that is, the exchange of gases between atmospheric air and the blood of the capillaries of the lungs is carried out by simple diffusion of gases through the alveolar-capillary membrane due to the difference in the partial pressure of oxygen in the inhaled air and venous blood flowing through the pulmonary artery into the lungs from the right ventricle. Compared to adults, young children have pronounced differences in external respiration due to the development of acini, numerous anastomoses between the bronchial and pulmonary arteries, capillaries.
Functional features.
Breathing depth in children it is much less than in adults. This is due to the small mass of the lungs and the structural features of the chest. The rib cage in children of the 1st year of life is, as it were, in a state of inhalation due to the fact that its anteroposterior size is approximately equal to the lateral one, the ribs from the spine depart almost at a right angle. This determines the diaphragmatic nature of breathing at this age. An overcrowded stomach and intestinal distention limit the mobility of the chest. With age, it gradually passes from an inspiratory position to a normal one, which is a prerequisite for the development of thoracic breathing.
Breathing rate the more, the younger the child:
newborn - 40-60 per minute;
infancy - 30-35 per minute;
older age - 15-20 per minute.
Breath type changes with age:
up to a year - abdominal;
1-7 years old - mixed;
From 7 years old - in boys, abdominal, in girls, chest.
Oxygen demand in children it is much higher than in adults. So, in children 1 year of life, the need for oxygen per 1 kg of body weight is about 8 ml / min, in adults - 4.5 ml / min. The superficial nature of breathing in children is compensated by a high respiratory rate. Due to the higher frequency, the minute volume of respiration per 1 kg of body weight is two times higher in young children than in adults. The vital capacity of the lungs (VC), that is, the amount of air (in milliliters) exhaled maximum after maximum inhalation, in children is significantly lower than in adults. VC increases in parallel with the growth of the volume of the alveoli.
Thus, the anatomical and functional features of the respiratory system in children create the prerequisites for easier breathing disorders than in adults.
The respiratory system of a newborn, like all other systems of a newly born baby, is still imperfect. The lower nasal passage is not developed, the glottis is much narrower than in adults, the pharynx is underdeveloped, the bronchi are narrower, and the trachea has a too narrow lumen. All respiratory organs of newborns have yet to be finally formed, and until this happens, parents should be extremely careful.
Anatomical and physiological features of the respiratory system of a newborn child
In the prenatal period, the lungs are in a collapsed state. At the moment of birth, the child makes the first breathing movement, which we learn about thanks to the first exhalation - a cry. Breathing becomes possible thanks to a special substance - a surfactant that covers the walls of the alveoli already in the prenatal period. The surfactant prevents the collapse of the alveoli and the development of respiratory disorders during the neonatal period.
The upper respiratory tract in an infant has a number of features: the nose is wide and short, the lower nasal passage is not developed, the mucous membrane is delicate and easily wounded. The baby may have difficulty breathing due to blockage of the nasal passages during the inflammatory process, this makes him breathe through his mouth.
Another anatomical and physiological feature of the respiratory system of a newborn is the underdevelopment of the frontal and main groove, they begin to mature only after 1 year of life.
The baby's pharynx is narrow, the lymphatic glands forming a ring in it are underdeveloped, the tonsils are small. In this regard, children of the first year of life do not have sore throats.
The respiratory organ of a newborn, such as the larynx, has a funnel-shaped shape. The vocal cords are short, the glottis narrower than in adults. The mucous membrane of the larynx is delicate, well supplied with blood vessels and lymphoid tissue. Due to these features, babies often develop laryngeal stenosis. Children have a clear voice due to short vocal cords. At 3 years of age, the size and shape of the larynx in boys and girls are the same. Sexual differences are formed by the period of puberty and are associated with the fact that in boys the angle of intersection of the thyroid cartilage becomes sharper, the vocal cords are lengthened.
The trachea has an almost funnel-shaped shape and a narrow lumen, its cartilage is very pliable and easily displaced. The number of mucous glands is small. This anatomical and physiological feature respiratory system newborns contributes to the development in it inflammatory processes and the occurrence of stenosis.
The bronchi are narrow, the cartilage in them is soft. A special feature is that one bronchus - the right one - occupies a vertical position, being a continuation of the trachea, the left one departs at an angle from the trachea. Foreign bodies more often fall into the right bronchus. There are few mucous glands in the mucous membrane of the organ, but it is richly supplied with blood. All these features of the respiratory organs of young children contribute to the easy occurrence of inflammatory processes and stenotic complications.
The baby's lungs are in constant development. During the neonatal period, they are less airy, abundantly supplied with blood vessels, their elastic tissue is not sufficiently developed. After the birth of the world, the number of alveoli in the respiratory system of a newborn child increases and continues to grow up to 8 years.
Features of the respiratory system of young children: respiratory rate
During the first months of life, breathing is changeable, an increase in its rhythm can be observed. In infancy, breathing is shallow, due to the horizontal position of the ribs, weak contraction of the diaphragm, and the relatively large size of the liver. All this contributes.
The respiratory rate decreases with age: in a newborn it is 75-48 per minute, in the first year of life it is 45-35. The ratio between breathing and heart rate in newborns is 1: 3, later - 1: 3.5-4.
Respiration in children is counted with a hand placed on the chest or abdomen, in restless children - on the eye.
In infants in the first months of life, breathing is counted through a stethoscope attached to the baby's nose. Breathing disorders in children can occur:
- with inflammatory edema of the bronchial mucosa as a result of a decrease in their lumen;
- with the accumulation of sputum in the respiratory tract;
- with spasm of the muscles of the bronchi, leading to respiratory failure;
- by inhalation of foreign bodies;
- with compression of the airways;
- against the background of respiratory tract diseases. Respiratory disorders require the use of emergency measures.
Anatomical, physiological and functional features of the respiratory system in newborns explain the significant incidence of diseases, especially pneumonia, and their more severe course during infancy.
Article read 2,122 times (a).
All airways in a child are significantly smaller and narrower than in an adult. The structural features of children in the first years of life are as follows: 1) thin, easily injured dry mucous membrane with underdevelopment of the glands, reduced production of immunoglobulin A and surfactant deficiency; 2) rich vascularization of the submucosal layer, represented by loose tissue and containing few elastic elements; 3) the softness and pliability of the cartilaginous framework of the lower respiratory tract, the absence of elastic tissue in them.
Nose and nasopharyngeal space small size, the nasal cavity is low and narrow due to insufficient development of the facial skeleton. The shells are thick, the nasal passages are narrow, the lower one is formed only by the age of 4. Cavernous tissue develops by the age of 8 - 9, therefore, nosebleeds in young children are rare and caused by pathological conditions.
Paranasal sinusesonly the maxillary sinuses are formed; the frontal and ethmoid are open protrusions of the mucous membrane, taking shape in the form of cavities only after 2 years, the main sinus is absent. Completely all paranasal sinuses develop by the age of 12-15, but sinusitis can develop in children of the first two years of life.
Nasolacrimal duct. Short, its valves are underdeveloped, the outlet is located close to the corner of the eyelids.
Pharynx relatively wide, palatine tonsils at birth are clearly visible, their crypts and vessels are poorly developed, which explains the rare diseases of angina in the first year of life. By the end of the first year, the lymphoid tissue of the tonsils is often hyperplastic, especially in children with diathesis. Their barrier function at this age is low, like in lymph nodes.
Epiglottis. In newborns, it is relatively short and wide. The incorrect position and softness of its cartilage can cause functional narrowing of the entrance to the larynx and the appearance of noisy (stridor) breathing.
Larynx is higher than in adults, sinks with age, is very mobile. Its position is unstable, even in the same patient. It has a funnel-shaped shape with a distinct narrowing in the region of the subglottic space, bounded by the rigid cricoid cartilage. The diameter of the larynx in this place in a newborn is only 4 mm and increases slowly (6 - 7 mm at 5 - 7 years old, 1 cm by 14 years), its expansion is impossible. The thyroid cartilage in young children forms an obtuse angle, which becomes more acute in boys after 3 years. From the age of 10, the male larynx is formed. True vocal cords in children are shorter, which explains the pitch and timbre of the child's voice.
Trachea. In children of the first months of life, the trachea is often funnel-shaped; at an older age, cylindrical and conical shapes predominate. Its upper end is located in newborns much higher than in adults (at the level of IV and VI cervical vertebrae, respectively), and gradually descends, like the level of tracheal bifurcation (from III thoracic vertebra in a newborn to V-VI at 12-14 years old). The tracheal framework consists of 14-16 cartilaginous half-rings, connected behind by a fibrous membrane (instead of an elastic end plate in adults). The child's trachea is very mobile, which, along with the changing lumen and softness of the cartilage, sometimes leads to a slit-like collapse of it on expiration (collapse) and is the cause of expiratory shortness of breath or rough snoring breathing (congenital stridor). Stridor symptoms usually disappear by age 2, when the cartilage becomes denser.
Bronchial tree to the birth is formed. The number of branches does not change with growth. They are based on cartilaginous half rings, which do not have a closing elastic plate, connected by a fibrous membrane. The cartilage of the bronchi is very elastic, soft, springy and easily displaced. The right main bronchus is usually an almost direct continuation of the trachea, therefore it is in it that foreign bodies are more often found. The bronchi and trachea are lined with cylindrical epithelium, the ciliated apparatus of which is formed after the birth of the child. Bronchial motility is insufficient due to underdevelopment of muscles and ciliated epithelium. Incomplete myelination of the vagus nerve and underdevelopment of the respiratory muscles contribute to the weakness of the cough impulse in a small child.
Lungs have a segmental structure. The structural unit is the acinus, but the terminal bronchioles do not end in a cluster of alveoli, as in an adult, but in a sac. From the "lace" edges of the latter, new alveoli are gradually formed, the number of which in a newborn is 3 times less than in an adult. The diameter of each alveolus also increases (0.05 mm in a newborn, 0.12 mm at 4-5 years, 0.17 mm by 15 years). At the same time, the vital capacity of the lungs increases. The interstitial tissue in the child's lung is loose, rich in blood vessels, fiber, contains very few connective tissue and elastic fibers. In this regard, the lungs of a child in the first years of life are more full-blooded and less airy than that of an adult. Underdevelopment of the elastic frame of the lungs contributes to both the occurrence of emphysema and atelectasis of the lung tissue. The tendency to atelectasis is enhanced by surfactant deficiency. It is this deficit that leads to insufficient expansion of the lungs in premature infants after birth (physiological atelectasis), and also underlies the respiratory distress syndrome, which is clinically manifested by severe DN.
Pleural cavity easily extensible due to the weak attachment of the parietal leaves. The visceral pleura, especially relatively thick, loose, folded, contains villi, most pronounced in the sinuses and interlobar grooves. In these areas there are conditions for a more rapid emergence of infectious foci.
Lung root. Consists of large bronchi, blood vessels and lymph nodes. The root is an integral part of the mediastinum. The latter is characterized by slight displacement and is often the site of development of inflammatory foci.
Diaphragm. Due to the peculiarities of the chest, the diaphragm plays an important role in the breathing mechanism in a small child, providing a depth of inspiration. The weakness of its contractions explains the shallow breathing of the newborn.
Main functional features:1) the depth of breathing, the absolute and relative volumes of the respiratory act are significantly less than in an adult. When crying, the volume of respiration increases 2 - 5 times. The absolute value of the minute volume of respiration is less than that of an adult, and the relative value (per 1 kg of body weight) is much larger;
2) the younger the child, the higher the respiratory rate. It compensates for the small volume of the respiratory act. Rhythm instability and short apnea in newborns are associated with incomplete differentiation of the respiratory center;
3) gas exchange is carried out more vigorously than in adults, due to the rich vascularization of the lungs, blood flow rate, high diffusion capacity. At the same time, the function of external respiration is disturbed very quickly due to insufficient excursions of the lungs and expansion of the alveoli. Tissue respiration is carried out at a higher energy expenditure than in adults, and is easily disturbed with the formation of metabolic acidosis due to the instability of enzyme systems.