Urogenital infections are a combined group of sexually transmitted inflammatory diseases (STDs). As a rule, these are the pathologies that penetrate the body of women and men during unprotected (vaginal, anal, and more often oral) sex with an infected partner. In rare cases, infections such as chlamydia and syphilis can be transmitted in the home, during blood transfusion, using non-sterile syringes, as well as during natural childbirth, during the passage of the fetus through the birth canal. In this article, we will dwell on the types of urogenital infections, as well as talk about the diagnosis of these diseases and their treatment.
Types of urogenital infections
The infectious diseases under consideration differ depending on the microorganisms that cause them. It can be enterococci and staphylococci, mycoplasmas and ureaplasmas, gardnerella or chlamydia, herpes virus or a fungus of the genus Candida. As a result of their penetration into the body, such diseases develop as:
- mycoplasmosis;
- ureaplasmosis;
- trichomoniasis;
- chlamydia;
- cytomegalovirus;
- gardnerellosis (bacterial vaginosis);
- papillomavirus infection;
- candidiasis (thrush).
Consider the causes and signs of each urogenital infection.
1. Mycoplasmosis
This is an infection that is caused by an intracellular microbe called mycoplasma. As a rule, it occupies the urethra, cervix and vagina of a woman, as well as the foreskin of a man. However, women who are sexually promiscuous are more likely to suffer from mycoplasma.
There are 14 types of mycoplasmas that can provoke: pyelonephritis and prostatitis, urethritis and postpartum endometritis, adnexitis and salpingitis, salpingo-oophoritis, as well as pathologies of pregnancy and fetus.
The insidiousness of mycoplasmosis is that this infection practically does not manifest itself in any way. True, under certain conditions, men can feel uncharacteristic discharge in the morning and a pulling pain in the groin. And women suffering from mycoplasmosis may experience profuse discharge between periods and pain during intercourse.
Mycoplasmosis is especially dangerous for pregnant women, in whom this infection can cause:
- the threat of termination of pregnancy;
- abnormal attachment of the placenta;
- complicated pregnancy;
- polyhydramnios;
- premature discharge of amniotic fluid;
- late toxicosis;
- premature birth.
Without adequate treatment, mycoplasmosis can cause infertility by interfering with the egg's ability to move.
2. Ureaplasmosis
This disease is often considered together with mycoplasmosis, since its causative agent, ureaplasma, like mycoplasma, belongs to intracellular microbes (an intermediate species between viruses and bacteria).
The risk factors that are most likely to be infected are:
- promiscuous sex;
- early onset of sexual activity (before 18 years);
- transferred STDs and gynecological pathologies;
- age from 14 to 29 years.
Such an infection is most dangerous for pregnant women, in whom it causes serious complications and can provoke premature birth.
3. Trichomoniasis
Such a disease of the genitourinary system causes the simplest unicellular - Trichomonas. Every year there are more and more patients with trichomoniasis, and girls and women aged 16–35 are at risk. In the United States alone, 3 million infected women appear annually.
Of the pathogenic factors contributing to the development of this ailment, one can single out:
- violation of the pH of vaginal secretions;
- deterioration of the epithelium;
- the presence of sexually transmitted diseases;
- frequent change of sexual partners.
Most often, the disease is transmitted from an infected person during sexual contact. In rare cases, infection occurs through the household, oral-fecal method, through food or when visiting a medical facility. Infection is also transmitted from animals.
The disease does not manifest itself for a long time. In men, pathology is detected earlier, as it begins to manifest itself with cuts during urination. In women, trichomoniasis is manifested by frothy discharge, itching and burning, as well as the occurrence of cervical erosion. Without treatment, it can cause infertility. If the expectant mother suffers from this infection, trichomoniasis can provoke premature birth or even fetal death.
 4. Chlamydia
4. Chlamydia
This infection can develop on any mucous membrane that is covered with columnar epithelium. At the same time, chlamydia that multiplies in the body for a long time does not cause absolutely any symptoms. Most often, a woman finds out about this ailment at the moment when chlamydia provokes the development of another infectious disease, for example, such as: cervicitis and bartholinitis, salpingitis, urethritis or salpingo-oophoritis.
Depending on the ailment caused, the symptoms of infection also vary. For example, salpingitis manifests itself as pain in the lower abdomen, uncharacteristic discharge and subfebrile temperature, salpingo-oophoritis - pain in the sacrum and bleeding between menstruation, urethritis - increased urge to urinate and itching in the urethra, and bartholinitis - inflammation of the Bartholin gland and the appearance of an infiltrate. However, most often chlamydia provokes the development of cervicitis, which manifests itself as bleeding during the intermenstrual period and mucopurulent discharge from the vagina.
The development of chlamydia in pregnant women is extremely dangerous, as it can cause:
- undeveloped pregnancy;
- ectopic pregnancy;
- weak labor;
- premature placental abruption;
- gestosis;
- polyhydramnios;
- intrauterine fetal hypoxia.
Chlamydia in men also remains undetected for a long time, manifesting itself only in the case of the development of other infections, such as: urethritis and epididymitis, prostatitis and proctitis.
Usually men are overcome by urethritis, which manifests itself as pain and cramps during urination, as well as frequent urge. Complicating this inflammatory process often becomes prostatitis. In this case, pain in the groin, scrotum and sacrum is added to the symptoms that have already appeared, as well as bleeding during urination and bowel movements. If a man is struck by chlamydial epididymitis, he may experience pain in the testicle, which radiates to the sacrum or lower back, and if proctitis, it will be mild pain in the rectum, as well as mucous discharge.
5. Gardnerellosis
Bacterial vaginosis (gardnerellosis) caused by gardnerella most often affects women of childbearing age. According to statistics, 20% of women worldwide suffer from this infection. Often, doctors find it in patients with purulent or chlamydial cervicitis.
Characteristic symptoms of bacterial vaginosis are white or gray foamy discharge, as well as a characteristic putrid (fishy) odor from the vagina. Moreover, the symptoms of the disease intensify before menstruation, as well as during intercourse. Other symptoms of gardnerellosis include itching in the vagina, a burning sensation and frequent urge to urinate.
A complication of this ailment can be pelvic inflammation, bartholinitis, urethral syndrome and infertility. And if a pregnant woman becomes infected with gardnerellosis, the infection can affect the developing fetus in the womb.
As for men, they are often only carriers of gardnerella, although in rare cases they can develop a chronic infection, for example, chronic prostatitis.
6. Human papillomavirus infection
The human papillomavirus (HPV) has more than 40 strains, each of which can affect mucous membranes and skin. Like other urogenital infections, HPV is more often transmitted through sexual contact, although it can enter the body even after touching the carrier of the infection. In this case, after the incubation period, nodular neoplasms (genital warts) appear on the human genitals.
These neoplasms rise above the surface of the skin, provoking aesthetic problems in the patient, as well as causing pain during sex. In addition, they can grow into the skin, causing pain. Finally, it is possible that the resulting papillomas will degenerate into cancer.
7. Candidiasis (thrush)
it infection causes the yeast-like fungus Candida, which enters the body when the immune system is weakened and the acid-base environment of the vagina changes.
Most often, this disease appears in women who complain to the doctor about itching in the perineum, as well as the appearance of whitish curd discharge, due to which the disease is called thrush. Moreover, the infection quickly spreads throughout the body, provoking the appearance of foci on the gastric mucosa and even in the human mouth.
At the same time, one should not think that thrush is an exclusively "female" disease. Candidiasis can also develop in men on the genitals and other mucous membranes.
8. Genital herpes
According to statistics, among sexually transmitted infections, urogenital herpes takes 3rd place. It is transmitted during intimacy with a person who is a carrier of the virus. Moreover, the disease actually does not have an acute course, and therefore, after a long period of incubation, a chronic course of the disease develops with periodic exacerbations.
Has genital herpes and characteristic symptoms. During periods of exacerbation, the patient develops itching in the genitals, and vesicles appear on the skin, which burst, turning into painful sores. If such a disease is not treated, it will gradually suppress the immune system, and in the future it may threaten men with impotence, and women with the inability to conceive a child or frequent miscarriages.
9. Cytomegalovirus
This is a conditionally pathogenic microflora, which peacefully "lives" in the body of 75% of the adult population of the planet. In addition to sexual contact, this infection is transmitted by airborne droplets, for example, by kissing. As in the case of genital herpes, the disease is more often chronic.
Cytomegalovirus infection is especially dangerous for the fairer sex. For pregnant women, such infection threatens with complications of bearing a fetus and a high probability of miscarriage. And during delivery, the infection can be transmitted to the baby, causing him to damage the genitourinary and nervous systems.
Diagnosis of diseases
You can identify an existing urogenital infection in three common ways that you will be offered in the clinic. It:
1. Delivery of bacteriological seeding (bacteriological seeding). As a rule, blood, urine or feces become the material for research. To prepare for this analysis, it is advisable to give up sexual intercourse 3 days before taking the tests, and also refrain from urinating and hygiene of the genitals in the morning before taking the tests.
2. Immunoassay analysis. Compared to bacterial culture, this is a more accurate analysis, through which an infectious agent can be identified at any stage of development (even in the incubation period). To do this, the patient donates venous blood, which means that a week before the procedure, you should refuse to take medicines, and the analysis itself should be taken on an empty stomach.
3. PCR (polymerase chain reaction). This is the most accurate method for detecting infections in the human body, which allows you to get the result in just a few days. The test material here is also blood, urine or feces, which means that the conditions for preparing for the test are similar.
Retinitis is an inflammation of the retina. Isolated retinitis is quite rare, and most often it is combined with damage to the choroid of the eye - choroid. Therefore, ophthalmologists often consider this pathology in the framework of chorioretinitis.
Table of contents:Retinitis reasons
There are two types of receptors in the retina: rods and cones. The former are responsible for peripheral and twilight vision, while the latter are responsible for visual acuity and color perception. That is why, when the retina is damaged, visual impairment occurs. 
As a rule, retinitis develops with hematogenous drift of infection from inflamed internal organs through the central artery. The retina is in close contact with the choroid of the eye, which is why the inflammatory process rapidly spreads from one membrane to another. In this case, they talk about the development of chorioretinitis.
Retinitis develops due to the following reasons:
- Infectious diseases of the body (tuberculosis, toxoplasmosis, syphilis,);
- Collagenosis (rheumatism);
- Allergic processes in the body;
- Blood diseases ();
- Endocrine diseases ();
- Hereditary factors (degenerative changes in the retina);
- Eye trauma;
- Intoxication;
- Ionizing radiation.

 The retina does not have sensitive innervation, which is why its damage proceeds without pain... First of all, the patient is worried about the deterioration of vision. With the localization of an inflammatory focus in the macula, central vision is impaired, as well as color perception. With damage to the periphery of the retina, the patient has a loss of visual fields, in addition, twilight vision is impaired.
The retina does not have sensitive innervation, which is why its damage proceeds without pain... First of all, the patient is worried about the deterioration of vision. With the localization of an inflammatory focus in the macula, central vision is impaired, as well as color perception. With damage to the periphery of the retina, the patient has a loss of visual fields, in addition, twilight vision is impaired.
Often with retinitis, patients are concerned about metamorphopsia, that is, the vagueness of objects and photopsies - the appearance of flashes before the eyes.
If untreated, inflammatory foci can transform into extensive scars, which leads to deterioration of vision.
 It occurs when pyogenic microorganisms from inflamed internal organs enter the retina. Metastatic retinitis develops with pneumonia, endocarditis, meningitis, sepsis (in particular postpartum). With septic retinitis, retinal vessels are damaged.
It occurs when pyogenic microorganisms from inflamed internal organs enter the retina. Metastatic retinitis develops with pneumonia, endocarditis, meningitis, sepsis (in particular postpartum). With septic retinitis, retinal vessels are damaged.
The disease can provoke the development of metastatic ophthalmia. With this disease, multiple whitish foci are formed on the fundus, located near the vessels. Inflammatory foci in the macular area often acquire a stellate shape. Gradually, the inflammatory process progresses, edema of the optic nerve head develops, while the vitreous dulls, its purulent fusion leads to panophthalmitis.
Viral retinitis
Caused by viruses, herpes. With the flu, retinal changes are observed quite often. First of all, the transparency of the retina is disturbed to varying degrees. So, in some patients, only a slight diffuse clouding of the membrane may be observed, while in others, the appearance of white spots of various sizes. Retinal opacity is caused by swelling of the interstitial substance.
The clouded areas resemble cotton wool, are located mainly in the macula, as well as around the optic nerve head. The vessels located in this area are not visualized.
Over time, the white spots diminish, become clearer, and then disappear. Vision is restored. However, the course of the disease often becomes recurrent. It is worth fearing exudative retinal detachment, as well as retinal pigmentary degeneration.
Cytomegalovirus retinitis
It is a slow-growing retinal infection that occurs in people with immunodeficiency disorders, particularly HIV. A slowly growing retinal focus is formed on the fundus, gradually covering all layers of the retina. As the inflammatory focus spreads, hematogenous retinal detachment may occur. Often the focus is located in the posterior pole, although the inflammatory process can be localized absolutely in any part of the retina.

Syphilitic chorioretinitis
This is a venereal disease caused by treponema pallidum. Infection of eye tissue with syphilis occurs in the second or third stage of the disease. Chorioretinitis is also found in children with congenital syphilis.
For congenital syphilitic chorioretinitis, the symptom of "salt and pepper" is characteristic, when on the periphery of the fundus there are many white foci, interspersed with dark foci. This sign persists throughout life.
With acquired syphilis, there are signs of diffuse chorioretinitis. There is edema of the retina and the optic nerve head; in the vitreous body there is a thin diffuse suspension in combination with rough floating opacities. In addition, retinal hemorrhages may occur. After the acute phase of syphilis subsides, multiple atrophic foci of the choroid, partially pigmented, are formed.
Toxoplasmotic retinitis
The development of retinitis is often associated with intrauterine infection. But it is worth noting that the symptoms of eye damage do not always appear at an early age.
With an inactive form of the disease, obsolete large atrophic or cicatricial chorioretinal foci with hypertrophy of the retinal pigment layer are found. The lesions are more often single than multiple, located in the posterior pole of the eye.
In the acute phase of toxoplasmosis, new inflammatory foci appear on the fundus, as well as along the edge of old changes. Exudative retinal detachment and retinal hemorrhages should be feared. ![]()
Tuberculous retinitis
When mycobacteria enter the eye, the choroid is primarily affected. With peripheral localization of the inflammatory process on the periphery of the retina, a corkscrew-like tortuosity of the vessels occurs, and along the venous wall there is an accumulation of fibrin in the form of a sleeve. Along the course of the veins, granulomas are visualized, which are elongated white foci. Hemorrhage occurs with the development of hemophthalmitis, which can provoke tractional retinal detachment.
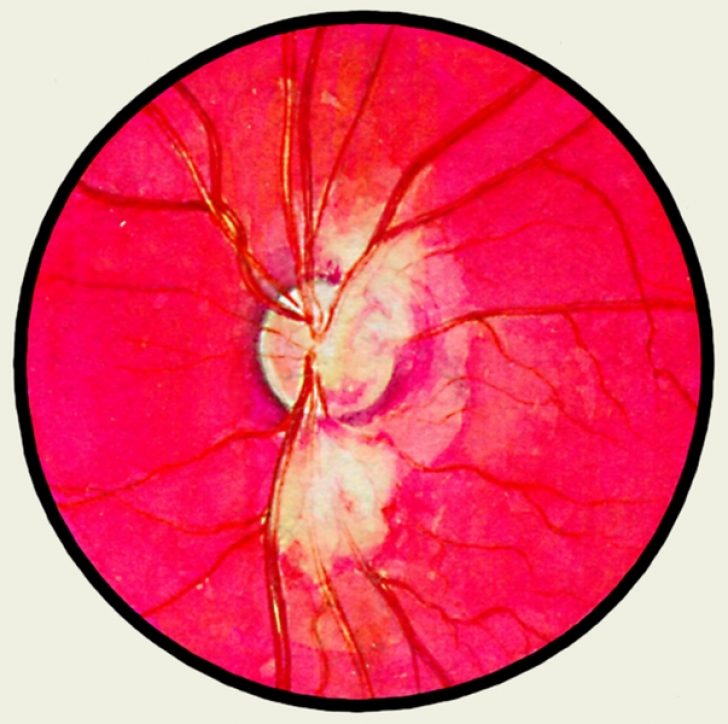 With this ailment, whitish muffs with jagged edges, located along the vessels, as well as perivascular banded retinal edema are noted on the fundus. In addition, hemorrhages may occur. If untreated, the vessels of the optic nerve head also suffer, which leads to visual impairment. Subsequently, in the area of \u200b\u200bthe disc, exudative foci of a star-shaped form are formed. In the absence of timely therapy, secondary perivascular fibrosis develops.
With this ailment, whitish muffs with jagged edges, located along the vessels, as well as perivascular banded retinal edema are noted on the fundus. In addition, hemorrhages may occur. If untreated, the vessels of the optic nerve head also suffer, which leads to visual impairment. Subsequently, in the area of \u200b\u200bthe disc, exudative foci of a star-shaped form are formed. In the absence of timely therapy, secondary perivascular fibrosis develops.
Retinitis pigmentosa
Retinitis pigmentosa is a dystrophic, not an inflammatory and infectious disease, but traditionally belongs to the group of retinitis. It is a hereditary, degenerative retinal disease associated with abnormalities in photoreceptors or retinal pigment epithelium.
The progression of the disease leads to the loss of a large volume of photoreceptors and, as a consequence, the possible development of blindness. The patient has the following symptoms:
- Night blindness;
- Lack of central or peripheral vision;
- Mesh vision;
- Blurred vision;
- Poor color discrimination.
With ophthalmoscopy, pigment deposits are determined in the form of so-called bone bodies, a decrease in the number and thickening of blood vessels, and waxy pallor of the optic nerve head.

Retinitis Coats
This is a fairly rare congenital disorder that causes partial or complete blindness. The causes are not known. It is characterized by abnormal development of blood vessels behind the retina. As a result, massive exudation and hemorrhages develop in the outer layers of the retina. So, between the retina and the choroid, exudate and blood are concentrated. These factors can lead to retinal detachment.
The disease is found in childhood or adolescence, more often among men. In most cases, one eye is affected. The patient is worried about blurred vision, blurred vision, photopsies. An interesting sign of ailment is the fact that in photographs taken with a flash, the sick person's eyes are yellow, not red. This is due to the reflection of light from the cholesterol deposits in the retina.
With ophthalmoscopy, cotton-wool foci without clear boundaries are visualized in the retina, as well as interrupted vessels. The lesions are often located near the macula or optic nerve head. As the disease develops, the foci enlarge, merge with each other. A characteristic feature is the presence of miliary aneurysms along the veins. 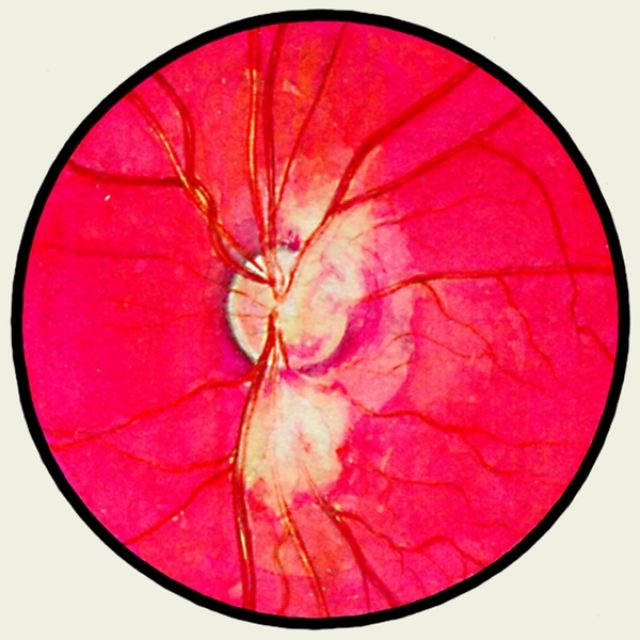
The causative agents of purulent infection are staphylococci, streptococci, Escherichia coli, gonococci, pneumococci, Pseudomonas aeruginosa and others in pure form or in association with each other (see the complete body of knowledge Pyogenic bacteria).
Due to the widespread use of antibiotics and their mutagenic action, the species composition of causative agents of purulent surgical infection has changed; the main place in it is occupied by staphylococcus (see complete body of knowledge) in monoculture or in various microbial associations. The change in the species composition of the microbial flora occurred simultaneously with an increase in its antibiotic resistance. As a result, the drug resistance of staphylococci isolated from patients with purulent infection to penicillin, streptomycin, chlortetracycline, chloramphenicol and erythromycin exceeds 70%, and often the microflora is multi-resistant - resistant to a large group of antibiotics under study.
The development of a purulent infection is determined by the interaction of a macro and a microorganism. An important factor is the nature, dose, virulence of the penetrated microbial flora, the state of the focus of the introduction of microorganisms - the presence of necrotic tissues that serve as a nutrient medium for microorganisms, the state of blood circulation, as well as the immunobiological characteristics of the organism.
Purulent infection occupies one of the main places in the surgical clinic, is the essence of many diseases and postoperative complications. Patients with pyoinflammatory diseases account for 1/3 of all surgical patients.
Most of the postoperative complications are associated with a purulent infection. According to the materials cited by Girhake and Schwick (F. W. Gierhake, H. G. Schwick, 1971), 42.5% of all deaths after surgical interventions are associated with purulent-inflammatory complications.
There is a certain dependence of the nature of pyoinflammatory diseases on the age of patients. At a young age (17-35 years), phlegmon (see full body of knowledge), abscess (see full body of knowledge), purulent lymphadenitis (see full body of knowledge), mastitis (see full body of knowledge), osteomyelitis (see full body of knowledge) are more common ); at the age of 36-55, diseases of the urinary system prevail - pyelitis, cystitis (see the complete body of knowledge), pyelonephritis (see the complete body of knowledge), paraproctitis (see the complete body of knowledge); over the age of 55 - carbuncle (see complete body of knowledge), necrotic phlegmon, post-injection abscess and others.
In children, purulent infection proceeds according to the type of neonatal phlegmon (see the complete body of knowledge of Phlegmon), sepsis (see the complete body of knowledge), suppurative diseases of the lungs and pleura, acute hematogenous osteomyelitis, staphylococcal peritonitis (see the complete body of knowledge).
Classification
Purulent infection is classified according to etiology, localization and clinical course. By etiology, monoinfection (staphylococcal, streptococcal, colibacillary, proteus, gonococcal, pneumococcal and others) and polyinfection (staphylococcal and colibacillary, staphylococcal and streptococcal and others) are distinguished. By localization, a purulent infection of the skin, subcutaneous tissue of the limbs and trunk is distinguished; the integument of the skull and its contents; neck; chest wall, pleura and lungs; mediastinum; peritoneum and abdominal organs; pelvis and its organs; bones and joints. Clinically, the course of a purulent infection can be acute general (sepsis), acute local (abscess, phlegmon, furuncle, carbuncle), chronic general (chroniosepsis), chronic local (abscess, empyema, osteomyelitis and others).
