prevention of acute respiratory diseases and acute respiratory viral infections , and factors of their prevention.
Humanity has coped with many serious and dangerous diseases. The terrible plague epidemics are a thing of the past, smallpox has been completely eradicated on the globe. However, respiratory infections are still common. viral infectionsknown in everyday life as influenza or flu-like diseases, and in medicine registered as ARI (acute respiratory disease) or ARVI (acute respiratory viral infection)
The number of acute respiratory infections is increasing. Two million lei was spent by the Buzau County Council for the renovation and supply of the hospital in the Parskovo commune.
- Doctors go outside again!
- Relatives of a 59-year-old woman who died of a stroke accused doctors of negligence.
- The young family claims that the doctors at the hospital treated her superficially.
So what's the deal here?
First of all,
Influenza is a widespread respiratory illness caused by a virus. It has characteristic symptoms in the form of intoxication of the whole body, chills and inflammation of the respiratory tract, and respiratory viruses, as their name implies, affect the upper airways and the lungs, therefore, the infection is spread by airborne droplets. This is the most “effective” way of spreading the infection. It is enough for one patient to start sneezing indoors, as viruses immediately begin to spread throughout the room and are actively inhaled by everyone in the room. Hence, the likelihood of infection of a large number of people is high. The causative agent of influenza was discovered in 1933 by the English virologists W. Smith, F. W. Andrews, P. Laidlaw
The second half of the class consists of children who are hardly affected by virginity, which makes their head all over the school. What is the explanation for this phenomenon? Why are only some of the children affected while the rest are not even bothered by the existence of virosis?
The story above occurs even as you read these lines in the middle of eight years of college. This is not the first time this phenomenon occurs, we had the same situation with the scarlet one, which scared us very much. As a rule, in such situations, doctors recommend that all children in the community receive treatment so that the virus is completely destroyed, so that the area is decontaminated as soon as possible. The idea is that some babies, even if they are not sick, may be carriers of the fetus.
As a result of influenza disease, the body temperature rises sharply, and remains within 38-40 ° C. In this case, a person feels increasing pain in the muscles and head, fatigue. With illness, the nasopharynx is dry, there is no discharge from the nose. A little later, there is a dry, hacking cough that radiates to the sternum.
Secondly,
The spread of respiratory viral infections is facilitated by the intensive development of communications, air traffic, road and rail transport. A patient with influenza can cover a distance of several tens of thousands of kilometers within a few hours, and, consequently, spread the infection over such a long distance. It is no coincidence that respiratory diseases began to spread widely inXX century and in XI distribution took on a large-scale character.
Still, why weren't some of the children hurt? What difference does it make if they are so stable? Immunity is the key, everyone knows, but how does she understand it? Can anyone provide a winning recipe for kids to boost their immunity and not get so bad and so often?
Over time, we have found very few links, most of them are recent. In short, the information provided by the doctor is as follows. This is a way of protecting the body from various diseases, among which the most dangerous are infectious diseases. These protective actions are carried out by organs, tissues and cells, which together make up the immune system.
Thirdly,
The spread of respiratory viral infections is facilitated by the relative ease of the disease, as a result of which the sick are not hospitalized or isolated from others, many of them consider it possible to go out and use public transport.
Fourth,
The body lacks sufficiently effective mechanisms to combat respiratory viruses. Immunity is developed within a week (hence the average duration of acute respiratory viral infections), but it is not very long-lasting (within a few weeks). And most importantly, viruses of respiratory infections are characterized by variability (mutation, adaptation of antigenic properties), which does not allow preparing a vaccine that would be suitable for repeated epidemics of the virus of the same type. For example, the A (H1N1) virus in one epidemic is not identical to the A (H1N1) virus in the next epidemic. During mass epidemics (diseases), viruses meet a wide variety of conditions and have the opportunity to fully demonstrate their ability to transform antigenic properties.
This system is formed in the first years of life, so children and young children are more susceptible to recurrent diseases, especially respiratory diseases. Factors that cause a decrease in immunity. Read and: How We Encourage Children to Know Everything.
Another important risk factor for a reduced immune system is the child's environment. If a young person is exposed to secondhand smoke, polluted air, mold, moisture, all this leads to an increased risk of respiratory diseases. All of these factors cause constant irritation and inflammation of the mucous membrane, creating favorable conditions for contact with infectious microbes.
What helps to prevent respiratory viral infections?
Several factors contribute to the prevention of respiratory viral infections.
First factor
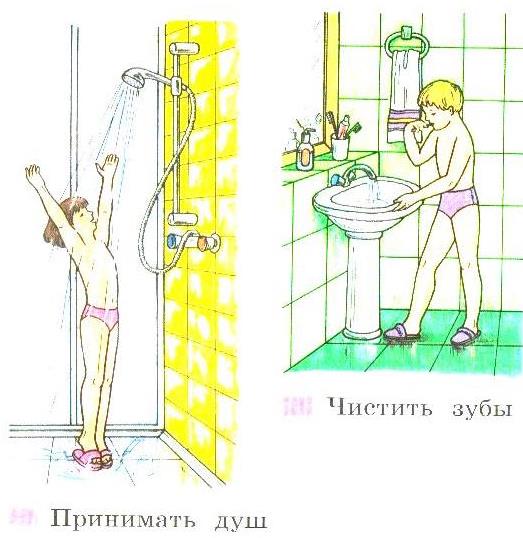
Health promotion is a clear and correct daily routine. A person should do not only what is necessary, which is directly prompted by his natural needs (eating, sleeping), but also what is good for healththe optimal combination of physical and mental work, proper nutrition, hardening and physical education, the correct alternation of work and active rest, good healthy sleep. Personal hygiene comes first in the fight and prevention of respiratory viral infections. Personal hygiene is about keeping your body clean.Personal hygiene is aimed at maintaining and improving health. Daily and periodic body hygiene is a high-quality hand washing after the street, before eating; washing; brushing your teeth 2 times a day; sharing a shower, washing the genitals; hardening. Periodic hygiene includes trimming the ends of the hair (every 4-8 weeks), trimming nails, shampooing hair, and prophylactic visits to the doctor.
Follow all the rules of personal hygiene and your life will be healthy, long and happy!
Recommendations for improving immunity. The most important doctor's recommendation is the importance of nutrition in the fight against infectious diseases. The child protection system is strengthened by components that play the role of immunomodulatory agents. It is very important to remember that the child is at risk by abandoning the natural diet.
All of these ingredients help to strengthen the body. The need for prebiotics is confirmed by their presence even in breast milk in the form of oligosaccharides. Household hygiene, personal hygiene, nutrition and diet play an important role in preventing various infections.
Due to a clear daily routine, the body, whether it is a child or an adult, experiences less stress, the expended forces are restored faster, the body wears out less.The body gets used to functioning in a certain daily routine, which has a beneficial effect on health in general. Healthy sleep is developed - you do not need to force yourself to fall asleep and wake up every time, since the body is already used to the regime. The daily routine for many people also includes a diet that is also very healthy. The daily routine allows you to plan your affairs in the most favorable way. So, in the first half of the day you can study / work, solve important matters and issues, and in the evening you can relax, devote time to your interests, hobbies and entertainment. The activity of a person who lives in a regime becomes more productive, he manages to do a lot.
See also: Colloidal silver is a natural antibiotic. The integration of milk into children's diets leads to a 10% reduction in infections in kindergartens, children with stronger immune systems and higher resistance to colds and infections. You have a wealth of information and professionals to help you make the best decisions for your child. Influenza is an acute viral respiratory infection caused by the influenza virus. Due to the rather serious complications of influenza that can lead to death, it should not be confused with a simple cold.
Presumptive daily routine for student productive activities.
Rise - 7.00
Morning exercises and washing - 7.00 - 7.30.
Breakfast - 7.30. - 8.00
Classes at school - 8.30 - 14.30.
Lunch - 14.30. - 15.00.
Walk in the fresh air - 15.00. - 16.00.
Preparation for school (implementation of D / C) - 16.00. - 18.00.
Sports activities - 18.00. - 19.00.
Influenza is transmitted through the air, but not only. More specifically, an infected person spreads around him sneezing, coughing, or even speaking, very small droplets of saliva or nasal secretions that are contaminated with the flu. If air containing these contaminated particles is inhaled by other people, contamination occurs. Another mode of transmission of influenza is through direct contact with the patient or patient's personal objects that are contaminated by their nasopharyngeal secretions.
It's good to know that the flu starts suddenly. This manifests itself in symptoms such as. High fever, weakness and physical exhaustion of muscles and joint pain, general shortness of breath. dry cough. rhinorrhea. headache... sore throat in the face of nausea and vomiting. What can we do to keep us safe from the flu?
Dinner - 19.00. - 19.30.
Free time - 19.30. - 20.30
Getting ready for bed (personal hygiene) - 20.30 - 21.00.
Sleep - 21.00. - 7.00
Second factor.
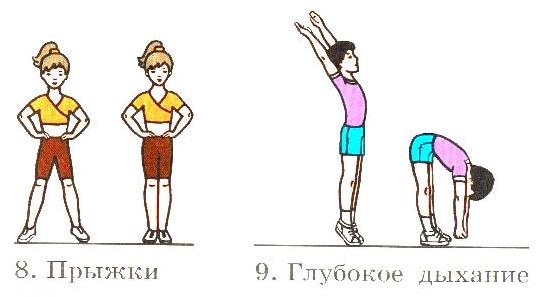
High physical activity, sufficient physical activity. Systematic physical education, daily morning exercises, which strengthens breathing, strengthens muscles, tunes the nervous system to the working mood, gives a boost of vivacity for the day, additional exercises in sports sections. It is very important to explain to students the importance and benefits of daily physical activity, it cannot be replaced by any special sports exercises. Schoolchildren who, after classes, during which they also sit, prefer to spend their free time at home at the computer, rather than on the street. Really modern schoolchildren have to spend less and less physical effort, the proportion of mechanical action is constantly decreasing. In addition, physical inactivity is a constant companion of people, the so-called sedentary professions of programmers, managers, etc.
Several preventive measures, including. Avoiding the crowd and the crowd. avoiding travel that covers your mouth and nose. in paper masks. knowing the flu symptoms. avoid contact with people with the flu. Wash your hands as often as water and soap, especially after visiting public places such as medical centers or pharmacies where people can be infected. strengthening of immunity. What should we do if we get the flu?
If we find that flu symptoms appear suddenly, we should take the following measures. Isolate at home to wear a protective mask that covers both mouth and nose, including at home. urgently advise the doctor to drink plenty of fluids, to calm down, to adhere to the symptomatic medication recommended by the attending physician. avoid automotive education. follow all the recommendations of your doctor. About 3-4 weeks if no other complications exist.
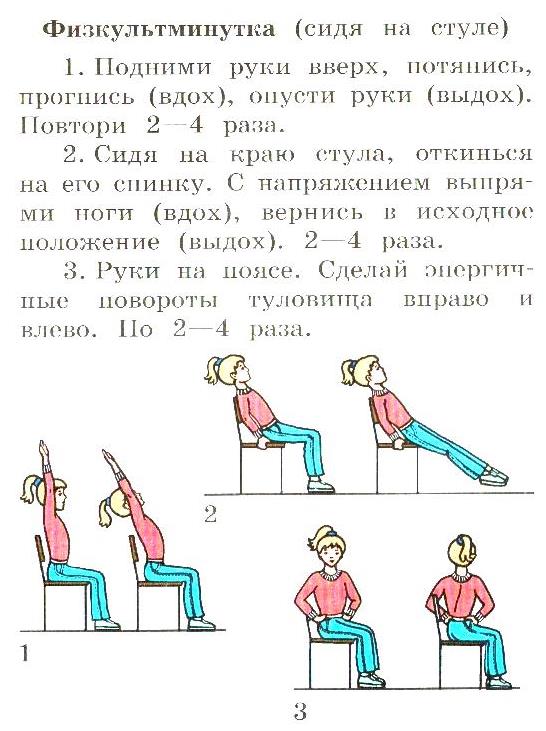
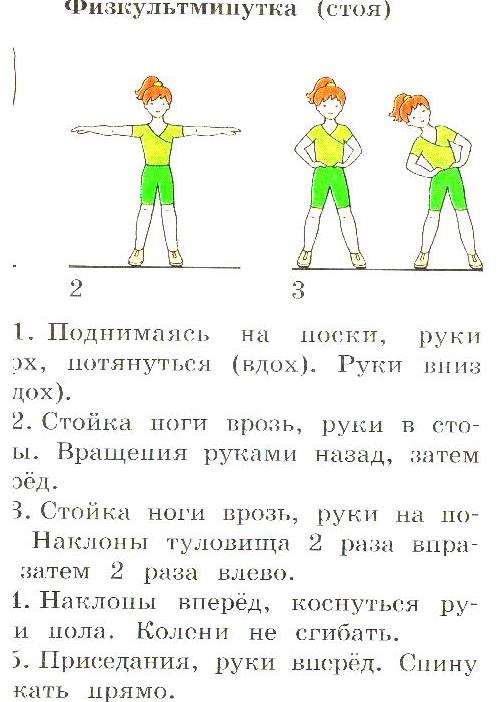
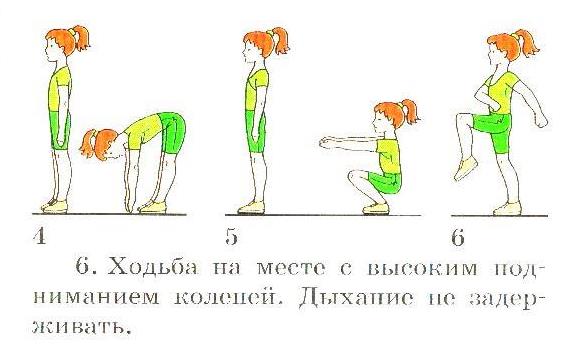
Approximate sets of exercises for Morning Exercise and physical education in the classroom.

What are the complications of influenza? Complications of influenza include: bronchitis, pneumonia, respiratory failure, myocarditis, meningoencephalitis, death. Is there a difference between swine flu and seasonal flu? No, there is no difference in terms of symptomatology and evolution. The only difference is in the structure of the virus, as the swine flu virus has another antigenic structure. It is known that the influenza virus rapidly changes its antigenic structure from one season to the next, creating a new virus strain.
It is for this reason that it is difficult to prepare an effective vaccine. So this is just another strain of the flu virus, except for the symptoms and development of the flu. In the case of a completely new virus, for which there is no immunity in the population, mortality may increase in the event of a pandemic. It also depends on the virulence of the pathogen, but also on the resistance of the organism to infection of the individuals concerned.
Regular breathing exercises contribute to the education of correct speech breathing with an extended gradual inhalation, the prevention of respiratory diseases. Breathing exercises are very useful in combination with aromatherapy or when working with a salt lamp. The salt lamp is an excellent decoration for a room and a solution to the problem at home with an increase in immunity. Such devices are made of rock salt. It is enough to turn on a light bulb or light a candle, and salt ions will fill the room in which you breathe. Its soft, calm light is aimed at strengthening the immune system. It can work all the time when you are in the room. The healing power of salty air for enhancing immunity has been proven many centuries ago.
Is swine flu spread by eating pork? Swine flu is not spread by roast pork. It is spread by air or direct contact with the patient or objects contaminated with their own secretions. This article was written in collaboration with Dr. Mogosan Ioan-Marius.
Prevention of acute avian bolus includes prophylactic specifics. A very balanced diet, including more vegetables and fruits, and avoiding crowded places, as possible, rinsing your nose, small hands hygiene, etc. Specific is the vaccination of the child against influenza and the introduction of immune drugs. It is not recommended to work too much with immunity drugs, because their echo is not always predictable. Vaccination of young children is recommended, because they are exposed to worse, more aggressive forms in case of illness.

Proper breathing stimulates the heart, brain, and nervous system. The ability to control breathing allows you to control yourself. A slow exhalation helps to relax, calm down, and cope with anxiety and irritability.
"Big Sea" - and. by. from. (3-4 times)
It is recommended to vaccinate infected children with chronic diseasesbecause in the case of viral infections, they are most difficult to carry. The vaccine is applied only to a healthy child who has been well examined by a pediatrician before the vaccine. It is preferable to have a complete blood count and a complete urinalysis.
When it comes to caring for a sick child and a sick mature, it is very much like that. The child should be isolated, have a bed, a spouse and drink plenty of fluids. It is also not recommended to apply drugs to a temperature of 3 ° C-5 ° C, which is a fever, only a low-grade fever condition.
inhale, arms to the sides, rise on your toes.
exhale, return to and. P.
"Seagulls catch fish" - and. p. - legs apart. (3-4 times)
inhale, tilt forward, arms to the sides.
exhale, return to and. P.
Breathing exercises in combination with sea air are especially useful to breathe sea \u200b\u200bsalt, which is filled with air in the coastal zone. That is why doctors recommend at any time to visit sea resorts and breathe there with a reserve for the whole winter.
Two drugs for fever conditions: paracetamol and ibuprofen. But they are not used in combination. Paracetamol is preferably administered as a suppository. Ibuprofen is received after some data after 6 months or even in the first month. There is an interval between their use, repeated 6 hours. It is generally not recommended to use many drugs without a doctor's instructions.
If your child is doing well, do not immediately start lowering fever with antipyretics. The active ingredient is an extract of 200 K of wild and duck hearts energy, excipients are sucrose and lactose monohydrate. One dose contains 0.01 ml of extract.
There is a wide variety of breathing exercises that can be performed on the seashore
"Flower"
(according to B. Tolkachev's method)
Sitting in Turkish, closing your eyes, take a calm breath through your nose, hold your breath. On a long exhale, say "a - a - ah"
"The balloon rises up"
Research confirms the preventive effect of this product on symptoms acute infections upper respiratory tract and the therapeutic effects of influenza-like illnesses. Viral respiratory infections are an annual problem. Acute viral respiratory infections account for the largest proportion of infectious diseases... They damage not only human health, but also economic and social damage. Acute viral infections of the respiratory tract are airborne droplets and some of them, such as the flu, often cause serious complications.
Sit down in Turkish style, with one hand between the collarbones.
1. Calm inhalation with slow lifting of the shoulders.
2.Exhale calmly, shoulders drop
Repeat 3 times.
"Balloon"
(according to B. Tolkachev's method)
Lying on your back, legs are freely extended, eyes closed, palms on the stomach.
1. Slow inhalation - only the stomach rises.
In Lithuania, 100 thousand cases of influenza are registered annually, about 400 thousand. - other acute respiratory infections. The source of infection is a sick person or virus infected man. The infection spreads through the air and through contaminated household items and hands. The virus spreads all year round, but more often in winter. Excessive illness generates immunity only for a certain sero-reserve.
Affects the respiratory tract for both animals and humans. It is associated with symptoms of general hypertension, pneumonia, and severe breathing. Type A viruses are the most pathogenic for humans, cause the most severe diseases, develop epidemics and pandemics. Pediatric viruses do not cause epidemics; they do in some cases. The surface of influenza virus particles contains 2 antigens - hemagglutinin and neuraminidase. Because of their variability, influenza viruses change very quickly. Forms of variation of the influenza virus type "Ski-Riam-2".
2. Slow exhalation - the stomach goes down.
Repeat 3-4 times.

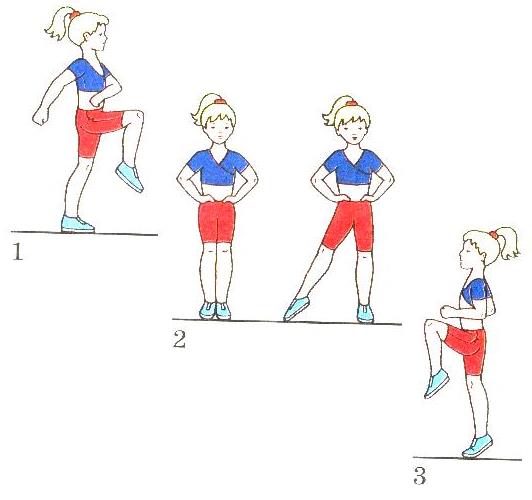
There are also several exercises to enhance breathing and blood circulation.
1. Walking in place.
2.Hands on the belt. Jump to the side of the right, then the left leg.
3. Running in place.
Third factor.
Hardening - strengthening health and constant communication with nature, the use of its favorable factors - fresh air, water, sun. Take time to walk every day. Clean and fresh air contains sufficient oxygen for the body, promotes vigor, active mood and high efficiency. Unfortunately, many people, including students, have not developed the need to breathe fresh air. Daily dousing with water or rubbing down leads to "accustoming" the body to the effects of cold and other unfavorable factors. The most common type of hardening is bathing. Sea bathing is especially useful, due to the complex effect on the body of temperature, special composition of water, and sunlight. Fresh air, wind, smell. Swimming in the sea or river is inseparably compatible with sunbathing
There are several ways to harden with water: rubbing, dousing, taking a contrast shower. You need to start hardening with water by wiping cold water... For this procedure, you must have a dry towel, sponge or special mitt and a bowl of water. After moistening with water and slightly squeezing the sponge, you should wipe the body in the following sequence: each hand - from fingers to shoulder; neck, chest and abdomen - from top to bottom; back - from the sides to the middle; each leg from toes to thighs. Rubdowns should be done daily after morning exercises. It is important that the first day of the day the water in the basin should be at room temperature, the next every 2 - 3 weeks the water must be gradually reduced until it becomes the same as that of cold water flowing from the tap. After the procedure, it will be rubbed dry with a dry towel until slight redness and a feeling of warmth. Dousing is the next hardening stage after wiping, which must also be done in the morning after morning exercises. To do this, you need to undress and while standing in the bath, pour water from a basin on yourself. The water temperature should be approximately + 24 ... + 22 degrees. After a week, you can lower the temperature by 1 - 2 degrees and within a month, bring it to + 18 ... + 16 degrees. After graduation water treatments it is also necessary to rub it dry with a dry towel until slight redness and a feeling of warmth.
1 month1 - i
24 - 22
24 - 22
2 - 30
2 - i
22 - 20
24 - 22
40 - 60
3 - i
20 - 18
24 - 22
60 - 90
4th - i
18 - 16
24 - 22
90 - 120
Even short-term sunbathing is an excellent health-improving agent; they have a very complex and beneficial effect on the body: blood vessels expand, breathing deepens. It is scientifically established that hardened guys get sick three times less often. At the same time, the hardening of the body should take place daily, without missing a single day, since the body very quickly loses the "accumulated" hardening effect, so if there was a break that was long enough, you will have to start all over again.Regularly and gradually, these are the two most important rules of hardening. I would like to note that for a person who is weak, often ill, or who has suffered a severe illness, hardening especially needs to be started as early as possible, but at the same time very carefully. Every opportunity for hardening should be used to prevent acute respiratory illness. The whole environment should be tempered, including the air temperature in the room (22 - 18 degrees C). When the body gets used to it, it can be reduced to 17 - 16 degrees C. Doctors have established that air hardening occurs better if there is a barely noticeable air movement in the room. Those who are constantly tempered are not afraid of colds.
The fourth factor.
Correctly selected clothes, clothes for the season.
It makes no sense to wipe yourself with cool water, but at the same time sleep in an unventilated room wrapped in a duvet. It's the same with clothes,
Many boys and girls flaunt even in very cold weather without a coat or headdress. It would seem very good training, but then why are many of these daredevils more susceptible to respiratory infections and suffer from chronic rhinitis? The answer is very simple. During the lessons, they "soar" in warm clothes (the body overheats), and as soon as they go out into the street, there is a sharp hypothermia, which leads to an inevitable respiratory infection. It is extremely unhygienic to sit in leggings, a woolen jacket during lessons, and you also need to object to the fashion of walking without a hat (putting a hood over your head). The climate of our country and Western countries is very striking, temperature fluctuations are so striking that copying winter clothes is at least inappropriate. The consequences of such panache can be extremely dire.
Fifth factor.
Training the cold spots of the body.
You need to train your cold spots. For example, try to do without a scarf, or at least a warm one. Until the first frost, it does not need gloves. The throat should also be treated with cold point training; daily in the morning and in the evening it is necessary to gargle with cold water. If you start in the summer and continue in the fall, then by winter you can achieve the maximum effekthat. Probably many have noticed that if the legs are "chilled", a runny nose or a sore throat, they also need to be tempered.
To train the cold points of the feet, you need to start by walking around the house every evening without shoes and socks, for 1 - 2 minutes. Gradually increasing the time of walking barefoot up to 20 minutes, after which wash your feet with cool water gradually lowering the water temperature, in summer it is advisable not to miss the opportunity to walk barefoot, you need to start with the grass warmed up by the sun, and later go to damp ground. Even the poet A. Yashin wrote: "To wander on the damp earth - barefoot is a great happiness!" It is not for nothing that even in the old days in Russian villages, children were forced to run in the rain so that they would grow better. When taking air baths, it is necessary to strive for as much of the body as possible to "come into contact" with the air. Let it blow your arms, legs, back. On a warm summer day, it is advisable to expose your body to a gentle breeze. In the summer period, maximum lightness in clothing is allowed, of course, in compliance with the rules of decency and accepted norms of behavior.
All of these factors are links in the same chain for the prevention of acute respiratory diseases. And which of the following prevention factors colds choose whether an adult or a school student is free to decide for himself.We all want to be healthy and happy. But achieving this requires our efforts. Don't forget about your health, you can't buy health. You need to create it yourself: every day and at any age. One must firmly know that health is one of the most important life values \u200b\u200bof a person, his well-being and longevity. Explaining to students the value of health, one should pay attention to the fact that the foundations of health are laid from childhood, that any illness suffered in childhood affects the health of an adult.
The manual for doctors was created on the basis of the scientific and practical program of the Union of Pediatricians of Russia and the International Fund for Maternal and Child Health Protection "Acute respiratory diseases in children: treatment and prevention", developed with the participation of Pierre Fabre, GlaxoSmithKline, Servier [show] .
SCIENTIFIC AND PRACTICAL PROGRAM
"ACUTE RESPIRATORY DISEASES IN CHILDREN: TREATMENT AND PREVENTION"
PROGRAM LEADER
A. A. Baranov | academician of the Russian Academy of Medical Sciences, Professor, Chairman of the Executive Committee of the Union of Pediatricians of Russia, Director of the Scientific Center for Children's Health of the Russian Academy of Medical Sciences |
COORDINATORS |
|
A.V. Gorelov | professor, Moscow Medical Academy. I.M.Sechenova, Central Research Institute of Epidemiology, Ministry of Health of the Russian Federation, Moscow |
Kaganov B.S. | |
Korovina N.A. | professor, Russian Medical Academy of Postgraduate Education, Ministry of Health of the Russian Federation, Moscow |
Tatochenko V.K. | professor, Scientific Center of Children's Health, Russian Academy of Medical Sciences, Moscow |
Uchaikin V.F. | academician of the Russian Academy of Medical Sciences, |
EXPERT ADVICE |
|
Balabolkin I.I. | corresponding Member of the Russian Academy of Medical Sciences, Professor, Scientific Center of Children's Health, Russian Academy of Medical Sciences, Moscow |
Baleva L.S. | professor, Federal Center for Radiation Protection at the Research Institute of Pediatrics and Pediatric Surgery, Ministry of Health of the Russian Federation, Moscow |
Balyasinskaya G.L. | professor, Russian State Medical University, Moscow |
Blistinova Z.A. | leading Specialist, Moscow Health Committee |
Gavalov S.M. | professor, Novosibirsk Medical Academy |
Gorbunov S.G. | phD, Central Research Institute of Epidemiology, Ministry of Health of the Russian Federation, Moscow |
A.L. Zaplatnikov | candidate of Medical Sciences, Associate Professor, Russian Medical Academy of Postgraduate Education, Moscow |
Zeigarnik M.V. | |
Ilyin A.G. | ph.D., Ministry of Health of the Russian Federation, Moscow |
A.A. Korsunsky | professor, Ministry of Health of the Russian Federation, Moscow |
V.A. Proshin | head of Department, Moscow Health Committee |
Kharlamova F.S. | professor, Associate Professor, Russian State Medical University, Moscow |
Samsygina G.A. | professor, Russian State Medical University, Moscow |
Erdes S.I. | candidate of Medical Sciences, Associate Professor, Moscow Medical Academy. I.M.Sechenov |
Shilyaev R.R. | professor, Ivanovo State Medical Academy |
SCIENTIFIC EDITORS |
|
Zeigarnik M.V. | ph.D., Scientific Center of Children's Health, Russian Academy of Medical Sciences, Moscow |
Kazyukova T.V. | ph.D., Russian State Medical University, Moscow |
EXECUTIVE SECRETARY |
|
Safronova A.N. | candidate of Medical Sciences, Moscow Medical Academy. I.M.Sechenov, Moscow |
Chapter 9. Prevention of acute respiratory diseases
Key points:
- Taking into account the ways of spreading influenza and AR-VI, the isolation of a child from a sick person and a potential source of infection plays a leading role in the prevention of ARI.
- There are a number of effective vaccines against certain types of pathogens that cause acute respiratory infections: influenza, Hemophilus imfluenzae type b infection, pneumococcal infection.
- Bacterial vaccines against several respiratory pathogens based on ribosomal fractions of pathogenic bacteria or their lysates are widely used.
- One of the main methods of increasing a child's resistance to infectious agents is hardening.
- Interferon prophylaxis is indicated for children with a severe premorbid background, who are just starting to attend child care facilities, as well as for all children during a flu epidemic.
9.1. Exposure prevention
Exposure prophylaxis aims to prevent the child from coming into contact with the source of infection. Taking into account the ways of spreading influenza and ARVI, the isolation of a child from a sick person and a potential source of infection plays a leading role in the prevention of ARI. The main measures that can be taken in this regard are as follows:
- limiting child contacts during seasons of increasing respiratory morbidity;
- reducing the use of urban transport for travel with children;
- lengthening the time the child stays in the air;
- wearing masks by family members with signs of acute respiratory infections;
- thorough hand washing after contact with a patient with acute respiratory infections or items of care for him;
- limiting the attendance of children's institutions by children with fresh catarrhal symptoms. In the foci of acute respiratory infections, the following preventive measures are taken:
- quarantine is introduced for a period of 7 days from the moment of the last case of the disease, the sanitary and epidemiological regime is strengthened;
- wet cleaning of premises is carried out;
- patients with acute respiratory infections are isolated or hospitalized;
- contact persons are examined daily and thermometry is carried out;
- interferon prophylaxis and other methods of preventing acute respiratory infections are also carried out in the foci.
9.2. Dispositional prevention
The main methods of increasing a child's resistance to infectious agents are vaccination (also see below) and hardening. When the skin cools, there is a reflex narrowing of the blood vessels of both the skin and the nasal mucosa, which reduces the air temperature in the nasal cavity by 2 ° C. This disrupts the functions of protective cells, reduces the supply of antibodies, which increases the risk of infection. Hardening trains the reaction of blood vessels, in case of hardened during cooling, the air temperature in the nasal cavity drops by only 0.3-0.5 ° C.
Hardening does not require very low temperatures, the contrast of temperature and the regularity of the procedures are important. Effects on the soles of the feet, on the skin of the neck, lower back are well tempered, however, to obtain a uniform effect, it is better to influence the skin of the whole body. The maximum duration of cold exposure to a child should not exceed 10-20 minutes, its repetition and gradualness are much more important.
Hardening, if the child is kept in greenhouse conditions, will not give an effect, it is important to create a stimulating temperature environment: weather-appropriate clothing, normal temperature in the apartment (18-20 ° during the day and 2-4 ° C lower at night). Already from the 1st year, the child should be taught to walk (up to 4 hours a day), while avoiding excessively warm clothes.
It is necessary to start hardening from the first weeks of life - these are air baths during swaddling, gymnastics, before bathing. For this, the child is left undressed in the air for several minutes at a temperature of 22 ° C, followed by a gradual decrease to 20 ° C at the age of 2-3 months and 18 ° C by 4-6 months. For hardening, you should also use bathing: at the end of the bath, it is appropriate to pour water on the child with a temperature 2-4 ° C lower than the water in the bath, i.e. start with a temperature of 32-34 ° C, reducing it every 3 days by 2-3 ° C. At this rate of decrease in water temperature in a month, you can reach 18 ° C, and it should not be lower for an infant. After dousing the child, rub it with a towel.
Swimming of infants in the pool hardens not so much by itself (the water temperature in it usually does not fall below 26 ° C), but in combination with air baths before and after the pool.
In the second year, daily washing of feet with cool water can be added to dousing after a bath (2-3 times a week). Treatments begin with a water temperature of 27-28 ° C, reducing it every 1-2 days by 2-3 ° C to a final temperature of 15 ° C (slightly colder than room temperature).
A contrast shower has a good hardening effect: changing warm water (up to 40 ° C for 30-40 seconds) with cold (14-15 ° C) - extending its effect from 15-20 seconds to 30 seconds. To bring cold effects to unpleasant (i.e. apply too cold water or leaving the child under a cold shower for more than 30-40 seconds) is unacceptable - not because of a possible "cold", but because of the danger of causing a negative attitude of the child towards hardening. Any hardening procedure should evoke positive emotions, if the child is "shivering", is afraid, he should not be forced. It is not difficult for preschoolers to organize contrast air baths at home. To do this, in the child's bedroom before waking up, opening the transom, lower the temperature to 14-15 ° C, and then, waking up the child, they play with him with dashes from a warm room to a cold room.
A visit to the bath provides even more opportunities for contrasting effects, for children early age the temperature in the sauna should be around 90 ° C, the duration of the stay is gradually brought to 10 minutes, sitting on the 1st step. In the Russian bath, more than low temperatures (from 60 ° C with an exposure of 2-3 minutes, increase to 80 ° C for 6-8 minutes). During one session, children visit the steam room 2-3 times, in between they take a shower or air baths at room temperature or swim (slowly) in a pool with a water temperature of about 25 ° C.
Winter swimming, walking barefoot in the snow are unsafe types of hardening. If the parents conduct them, this should be done very gradually and the duration of the procedure should not be more than 40-60 seconds, since, having a large body surface area relative to the mass, the child cools much faster than an adult. The same can be said about dousing with cold water. For a preschooler, with a gradual decrease, it is quite possible to bring the water temperature to 8-10 ° C, although there is no need for this, the hardening effect will be good if you stop at 12-14 ° C. Cold dousing as a therapeutic measure should be strictly prohibited for a child with fever : Sudden cooling, leading to a sharp narrowing of the skin vessels, can be life-threatening.
Hardening after a mild ARI can be resumed (or started) after 7-10 days, in case of a disease with a temperature reaction duration of more than 4 days, in 2 weeks, and after a 10-day fever, in 3-4 weeks.
Does hardening reduce the incidence of SARS? It cannot completely protect against the disease when it comes into contact with a virus new to a child. However, the protection against infection in a hardened child is much more effective than in an unhardened child, so the number of respiratory diseases, especially more severe ones, will be much less.
9.3. Interferon prophylaxis
Interferons are widely used not only for treatment, but also for the prevention of influenza and acute respiratory infections of other etiology. Interferon prophylaxis is especially indicated for children with a severe premorbid background, who are just starting to visit child care facilities, as well as for all children during an outbreak of influenza.
Interferon preparations used to prevent ARVI:
- For prophylactic purposes, human leukocyte wasp-interferon is prescribed 5 drops 2 times a day in each nasal passage until the threat of infection ceases;
- Grippferon is administered to children from 1 year of age, 5 drops 2 times a day for 7-10 days;
- Viferon in candles at a dose of 15-500 thousand units. 1-2 times a day for 7 days, then 1 time a day, 2 times a week for 4 weeks.
9.4. Specific prevention of acute respiratory diseases
Vaccination against pertussis and measles has long become the basis for the fight against these infections, vaccination against influenza is being introduced more and more, but the large number of other pathogens of acute respiratory infections and their serotypes hinders the creation of effective universal vaccines.
Flu
The list of vaccinations of the Ministry of Health of the Russian Federation, carried out according to epidemiological indications, includes persons with high risk the development of influenza or its complicated course and death:
- persons over 60 years old;
- patients suffering from chronic somatic diseases, often suffering from acute respiratory infections, preschool children, schoolchildren;
- medical workers;
- workers in the service sector, transport, educational institutions;
- military contingents.
Vaccination is also recommended for the public as a method of personal protection against disease; with a 50-80% coverage of collectives, it can significantly reduce the incidence of influenza. The disease in vaccinated people is milder with a low risk of complications.
Specific prophylaxis is carried out by vaccines, which are prepared from the actual strains of viruses A / H 1 N 1 A / H 3 N 2 and B, recommended annually by WHO. For use in childhood subunit and split vaccines are recommended.
The following drugs are licensed in Russia:
- Grippol (Russia) is a subunit vaccine with an immunostimulant polyoxidonium. It is used in children from 3 years of age, adolescents and adults. Inject once subcutaneously in a volume of 0.5 ml (regardless of age) into the upper third of the outer surface of the shoulder;
- Agrippal S1 (Kyron Bering, Germany) is a subunit vaccine, administered intramuscularly to children over 3 years old and adults in 1 dose (0.5 ml), at the age from 6 months to 3 years - 1/2 dose (0.25 ml) ... Children who have not been vaccinated before are recommended to be vaccinated twice with an interval of 4 weeks; in subsequent seasons - 1 dose (0.25 ml for children under 3 years old and 0.5 ml for children over 3 years old);
- Begrivak (Kyron Bering, Germany) - split vaccine, used in the same way as Agrippal vaccine;
- Vaxigrip (Aventis Pasteur, France) - split-vaccine, administered subcutaneously or intramuscularly from the age of 6 months; children under 9 years old, if they have not previously been vaccinated and have not had influenza, are vaccinated twice with an interval of 1 month at a dose of 0.25 ml at the age of 3 years and at a dose of 0.5 ml at the age of 3 to 9 years; over the age of 9 years, vaccination is carried out once in a dose of 0.5 ml;
- Influvac (Solvay Pharma, Netherlands) is a subunit vaccine that is administered to adults and adolescents over 14 years old once (1 dose of 0.5 ml), children 6 months -3 years old - 0.25 ml, 3-14 years old - 0.5 ml; if children have not previously been vaccinated and have not had the flu, they are injected with 2 doses of the vaccine with an interval of 4 weeks;
- Fluarix (GlaxoSmithKline, Germany) is a split vaccine used in children over 6 months of age and in adults, including those with chronic pathology. It is administered subcutaneously or intramuscularly. Children over 3 years old are injected with 0.5 ml once, children under 3 years old - 0.25 ml twice with an interval of 4-6 weeks.
Immunity is developed 14 days after vaccination (for the Fluarix vaccine - after 10-12 days), it is short-term (6-12 months) and type-specific, which requires annual vaccinations. Prophylactic efficiency - 70-90%, the degree of protection in children and the elderly is slightly lower than in adults. When infected with other types of influenza virus, the disease is milder. A decrease in the incidence of acute respiratory viral infections in children vaccinated against influenza was noted.
Vaccination reactions and complications with the use of subunit and split vaccines are usually absent. Mild reactions are short-lived (48-72 hours), occur in no more than 3% of vaccinated people and are manifested by slight pain at the injection site.
Contraindications for all vaccines are an allergy to chicken egg proteins, to aminoglycosides (for vaccines containing them), allergic reactions to the administration of any influenza vaccine, acute diseases and exacerbations of chronic diseases (vaccination 2-4 weeks after recovery / remission), progressive diseases of the nervous systems. These vaccines are compatible with others (in different syringes).
Split and subunit vaccines can be used to vaccinate people with immune defects, pregnant and lactating women, and can be administered in conjunction with immunosuppressive therapy.
Hemophilus influenzae infection
According to the WHO recommendation, the vaccine against Hib infection is included in the schedule of vaccinations for infants in all developed and many developing countries. It has been shown that mass vaccination can reduce the incidence of both meningitis and severe bacterial pneumonia (by 20%). The WHO Regional Committee for Europe in 1998 set as one of the goals to reduce by 2010 or earlier the incidence of this infection in all countries of the region to less than 1 case per 100 thousand population. This vaccination, although not included in the National Calendar of Russia, is recommended by the Ministry of Health of the Russian Federation for use where there are opportunities for this.
Mass vaccination of children in the first months of life became possible after the development of protein-conjugated vaccines. In Russia, the Act-HIB vaccine is licensed, which is a capsular polysaccharide of H. influenzae type and conjugated with tetanus toxoid protein. The vaccine is combined with DTP in one syringe or separately, administered at a dose of 0.5 ml / m. Vaccinations are carried out starting from 3 months of age with an interval of 1-2 months, revaccination is carried out after 12 months. after the third vaccination. At the beginning of vaccination at the age of 6-12 months, 2 injections with an interval of 1-2 months are sufficient, and revaccination 12 months after the second vaccination. To vaccinate children aged 1 to 5 years, 1 injection of the vaccine is sufficient.
Vaccination reactions to Hib vaccines are mild and are manifested by hyperemia and induration at the injection site (less than 10% of vaccinated patients), low-grade fever is possible; a temperature above 38.0 ° C develops in no more than 1% of those vaccinated.
The vaccine has a high prophylactic efficiency (95-100%); the countries that introduced it have practically eliminated this infection. The duration of the detection of a protective antibody titer is at least 4 years. The Act-HIB vaccine has no special contraindications: it is not administered in case of hypersensitivity to any components of the drug, especially to tetanus toxoid. Vaccinations are not recommended when elevated temperature and acute infectious diseases.
Pneumococcal infection
The main difficulties in creating a vaccine are the presence of a large number (about 100) of Streptococcus pneumoniae serotypes and the low immunogenicity of polysaccharide vaccines in children under 2 years of age. The polysaccharide 23-valent vaccine Pnevmo 23 has been registered in Russia, which includes 90% of pneumococcal serotypes that cause severe diseases. It is used to protect children at risk of: over 2 years of age, with asplenia and a removed spleen, liquorrhea, lymphogranulomatosis, hemoglobinopathies, neutropenia, HIV infection, chronic renal failure, heart disease, diabetes and other conditions predisposing to pneumococcal infection. There are reports of the use of this vaccine in children over 2 years of age with recurrent diseases of the nasopharynx, middle ear and paranasal sinuses.
Pneumo 23 is injected once subcutaneously or intramuscularly, the inoculation dose is 0.5 ml for all ages. It causes the formation of immunity for 5-8 years. Revaccination (single injection of 0.5 ml) is recommended not more often than with an interval of 3 years. Complications are rare, and may be red and sore at the injection site lasting less than 48 hours.
In recent years, conjugated pneumococcal vaccines have been developed to protect young children; their widespread use is still constrained by their high cost.
Bacterial vaccines against multiple respiratory pathogens
Bacterial vaccines against several respiratory pathogens, created on the basis of ribosomal fractions of pathogenic bacteria (Ribomunil) or their lysates (Bronchomunal, IRS19), have become widely used. It has been proven that ribosomal fractions are more purified than lysed whole bacteria and more immunogenic (1 μg of ribosome is equivalent in its immunogenicity to 1 mg of lysate). The inclusion of Klebsiella pneumoniae membrane fractions in the composition of Ribomunyl as an adjuvant makes it possible to increase the severity of the antibody response by 5 or more times as compared with the isolated intake of ribosomes. Oral administration of Ribomunil leads to the contact of the antigens of pathogens contained in the ribosomes with macrophages located in the mucous membrane of the gastrointestinal tract, followed by their presentation to the lymphocytes of the MALT system (lymphoid tissue associated with mucous membranes). As a result, committed clones of B-lymphocytes appear, producing specific antibodies to the antigens of those pathogens whose ribosomes are contained in Ribomunil. In addition, the migration of committed B-lymphocytes from Peyer's patches to other lymphoid organs of the MALT system (palatine and pharyngeal tonsils, lymphoid formations of the respiratory tract, etc.) and their subsequent differentiation into plasma cells leads to the production of specific secretory IgA and the development of effective local immune defense against Streptococcus pyogenes, Streptococcus pneumoniae, Hemophilus influenzae and Klebsiella pneumoniae. Thus, oral administration of the ribosomal vaccine Ribomunil is accompanied by the induction of an antigen-specific antibody response from both local and systemic immunity. In a double-blind, placebo-controlled study, it was shown that the formation of specific antibodies while taking Ribomunil is statistically significantly higher than the body's response to the use of lysates and placebo.
It has been proven that therapy with Ribomunil is accompanied by a significant increase in the content of secretory IgA in bronchial secretions and a statistically significant increase in the titers of specific antibodies of the IgG and IgM classes to pathogens whose ribosomes are present in Ribomunil, in the tonsils. A statistically significant increase in the titers of specific antibodies of the IgA, IgM, IgG classes to the indicated pathogens in comparison with the initial values \u200b\u200band control is achieved in the blood serum by 24 days from the start of Ribomunil therapy and persists in the case of IgA, according to A.V. Karaulov, no less 12 months Thus, the use of Ribomunil leads to the active production of specific antibodies against the antigens of the most common pathogenic bacteria, the ribosomes of which are included in the preparation, and the creation of effective post-vaccination immunity, the duration of which is determined by the characteristics of the organism and the external environment, the age and lifestyle of children. According to N.A. Korovina, the average duration of the therapeutic effect after a three-month course of treatment with Ribomunil is 1.5-2 years. Ribomunyl causes positive changes in the cellular link of immunity, expressed in a significant decrease after 3 weeks of treatment in the number of CD4 + and a simultaneous increase in the number of CD8 + and CD3 + T-lymphocytes. After 6 months of treatment with Ribomunil, these positive changes in the immune response continue to increase, and there is a significant reduction in the indicators of cellular activation (a significant decrease in the amount of CD25 +, CD23 + and the level of beta-2-microglobulin).
Ribomunil is well tolerated and can be used in children of different age groups, does not have significant side effects (the most common is hypersalivation at the beginning of treatment, which does not require discontinuation of therapy) and can be combined with other vaccines and immunomodulators. In recent years, the possibility of combining it with the topical IRS19 vaccine produced as a nasal aerosol has been discussed. It is known that the combination of oral administration of Ribomunil with inhalation of nasal aerosol IRS19 can increase the effectiveness of treatment by 8% (94% of children suffer from acute respiratory infections less than 2 times within 12 months of observation). Thus, this combination may be of undoubted therapeutic interest.
In recent years, the possibility of the complex use of the ribosomal vaccine (Ribomunyl) and various influenza vaccines to increase the effectiveness of specific immunization of children has been actively studied. In Russia and abroad, an increase in the preventive effectiveness of vaccination against influenza in children from risk groups has been convincingly proven when vaccinations are carried out simultaneously with ribosomal immunization. According to V.F. Uchaikin et al. (2000), carrying out a full course of treatment with Ribomunil in combination with influenza vaccination leads to a 2.5-fold decrease in the incidence of ARVI compared with the group of children receiving only the influenza vaccine, and prevents the exacerbation of chronic diseases. According to N.A. Korovina (2000), the total incidence of influenza and acute respiratory infections was also lower in children immunized against influenza while using Ribomunil. Thus, vaccination of frequently ill children against influenza is characterized by a higher index of epidemiological effectiveness, especially when it is carried out during the period of receiving the ribosomal vaccine.
Reception of Ribomunil can be started at any stage of the infectious process, and the greatest therapeutic effect is achieved when the drug is used for at least 6 months. The effectiveness of ribosomal vaccination against ARI has been convincingly demonstrated in organized children's groups, in children with frequent and long-term illnesses, including those with chronic ENT and bronchopulmonary pathology, in patients in areas of environmental and radiation distress. The main effects of Ribomunil should be considered a statistically significant and significant reduction in the number of ARI episodes over 1-2 years, a decrease in the duration and severity of the course of infectious episodes, a pronounced reduction in the number of absenteeism by children to organized children's groups, a statistically significant sharp reduction in the need for antibiotic therapy, a decrease in the risk of development complications and repeated ENT and bronchopulmonary infections.
According to a meta-analysis that covered 14,213 patients in 11 countries of the world who received the ribosomal vaccine Ribomunil, taking the drug causes a significant decrease in the incidence of acute respiratory infections - on average 1.92 ± 0.25 episodes per person (versus 3.35 ± 0.41 episode in the placebo group); and the number of courses of antibiotic therapy - on average 1.70 ± 0.12 courses per person (versus 3.02 ± 0.44 courses in the placebo group).
Literature
- Guidelines for the Epidemiology of Infectious Diseases. Ed. V.I. Pokrovsky. M .: Medicine, 1993, vol. 1, 464 p.
- Titkova I.V. Prevention of influenza in healthcare professionals. Attending physician, 1999, No. 7, p. 38-39.
