To determine the height, frequency and duration of gastroesophageal refluxes in patients with GERD, intraesophageal pH-metry is performed. It also helps to find out the level of acidity of the stomach contents thrown into the esophagus. The severity of gastroesophageal reflux disease is determined using endoscopic examination ( esophagogastroduodenoscopy) the esophagus. This study allows you to establish various pathological changes ( edema and redness of the esophageal mucosa, ulcers, erosion, scars, etc.) on the mucous membrane of the esophagus.
With this pathology, heartburn, sour eructation, chest pain, nausea, vomiting, bloating, impaired appetite, a feeling of a lump in the throat are most often observed. Pain sensations, which are mainly localized behind the sternum, can radiate ( spread) in adjacent anatomically areas - the left shoulder, arm, back, neck.
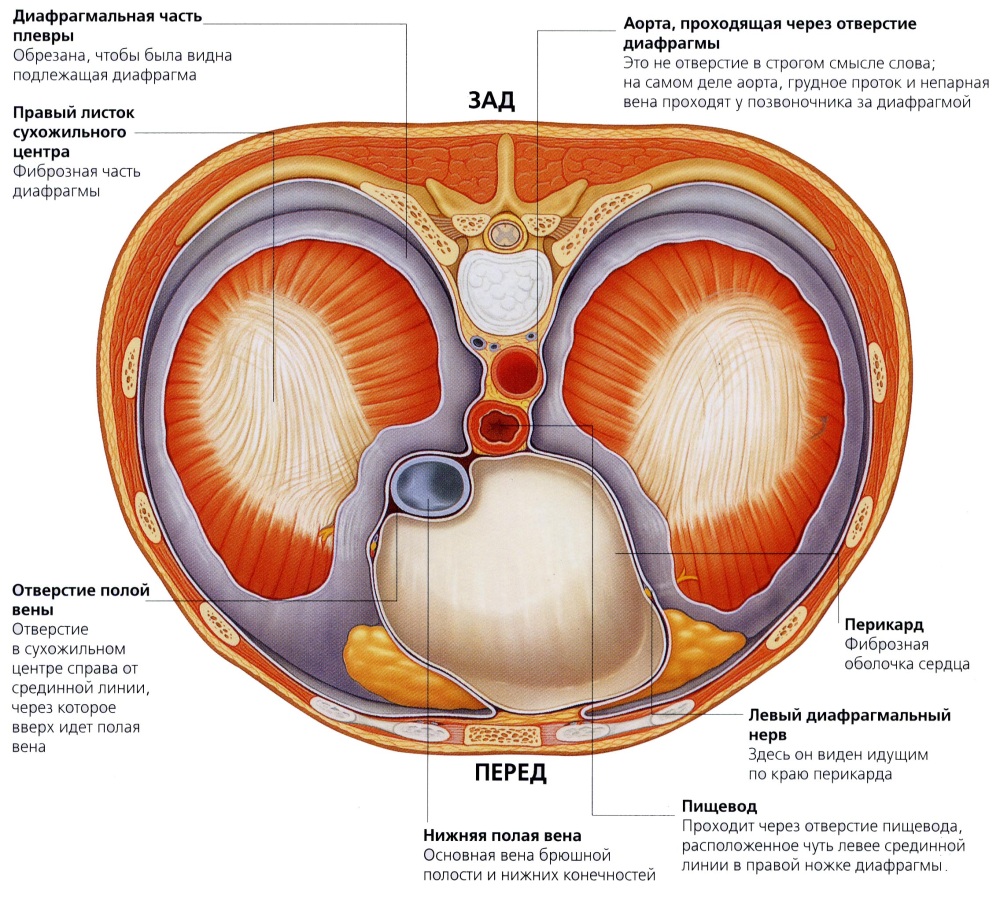
To confirm the diagnosis of hiatal hernia, such patients undergo contrast radiography, intraesophageal pH-metry, esophagomanometry, and endoscopic examination of the esophagus. Contrast radiography reveals pathological displacement of organs from the abdominal cavity to the chest cavity. Intra-esophageal pH-metry can confirm the presence of gastroesophageal refluxes and determine their characteristics ( duration, frequency, height).
Esophagomanometry is performed to assess the functioning of the esophageal peristalsis, which can be impaired with such a hernia. Endoscopic examination of the esophagus is necessary to identify pathological processes on its mucous membrane and assess the degree of its damage.
In addition to sour belching and heartburn with scleroderma, other signs may occur that indicate damage to the gastrointestinal system, such as dysphagia ( swallowing disorder), chest pain, abdominal pain, feeling of a lump in the throat, nausea, vomiting, weight loss, bloating.
Also, with scleroderma, patients may experience other symptoms, since scleroderma affects not only the gastrointestinal system. They can be pain in joints, in muscles, in the lower back, in the region of the heart, shortness of breath, cough, hoarseness, palpitations, pathological changes in the skin ( swelling, induration, whitening, etc.) and etc.
Scleroderma is characterized by leukocytosis ( an increase in the number of leukocytes in the blood), anemia ( decrease in the number of red blood cells in the blood) and an increase in ESR ( ) in a general blood test. From laboratory tests, such patients are also prescribed an immunological blood test for the presence of antinuclear factor, antibodies to the centromere and to Scl-70. Pathological changes occurring in the esophagus, stomach or intestines with scleroderma can be detected using contrast fluoroscopy and endoscopic examination of these organs.
With non-atrophic gastritis, patients usually have pain in the middle of the abdomen or in the epigastric region ( abdominal area below the sternum), sour belching, heartburn, nausea, vomiting. Pain syndrome most often appears with food intake and is not seasonal. The pain can be mild aching or, conversely, acute cramping. Painful sensations can appear on an empty stomach, however, in such cases, they are usually less pronounced.
For the diagnosis of non-atrophic gastritis, instrumental ( esophagogastroduodenoscopy, intragastric pH-metry) and laboratory ( cytological, immunological, microbiological, genetic) research methods. Esophagogastroduodenoscopy is an endoscopic examination that allows the doctor to visually assess the severity of inflammatory processes on the surface of the gastric mucosa. With non-atrophic gastritis, the gastric mucosa is usually shiny, red, slightly edematous, and may have minor hemorrhages, erosions, fibrin.
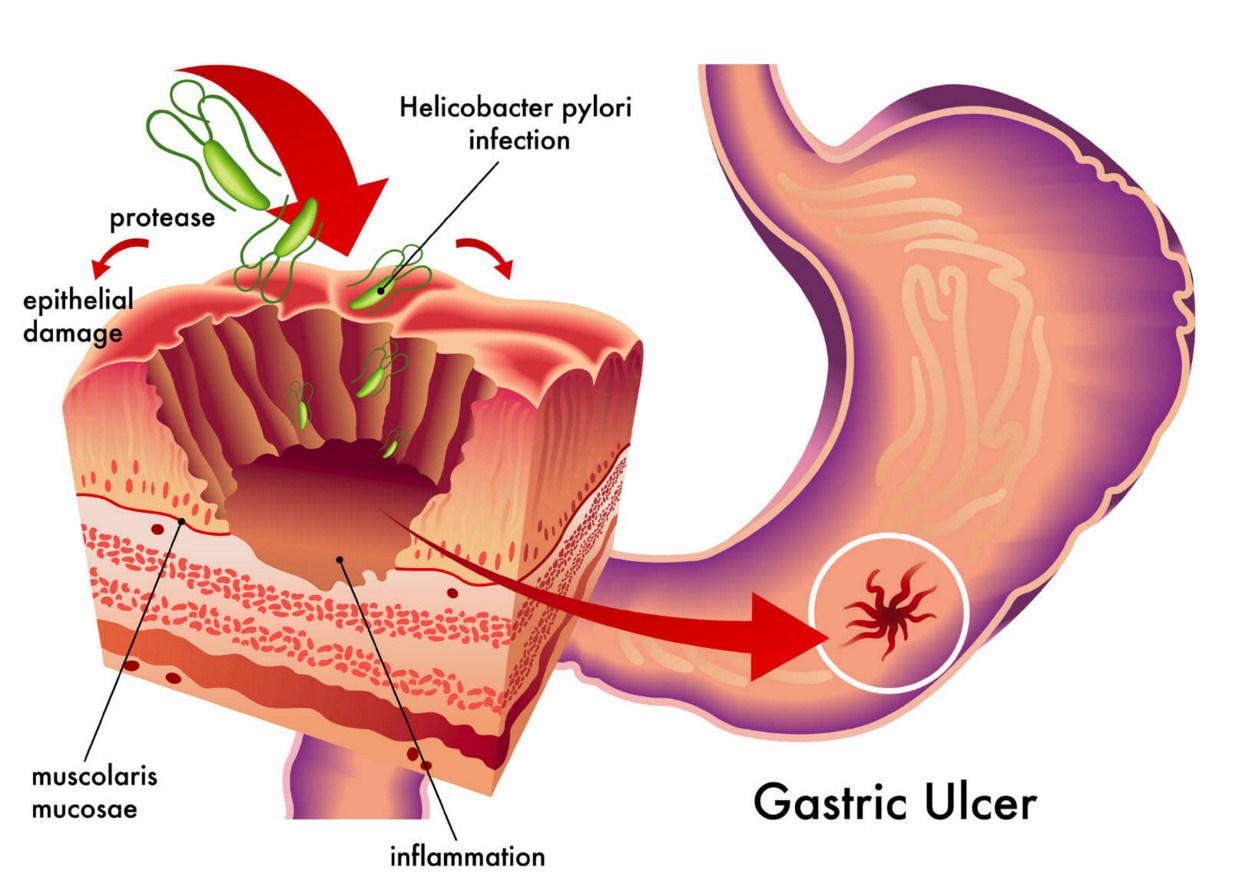
Intragastric pH metering is necessary to assess the acidity level inside the stomach. In non-atrophic gastritis, acidity is often increased. During the esophagogastroduodenoscopy, a piece of the mucous membrane of his stomach ( that is, take a biopsy). This piece of tissue is then delivered to the laboratory and examined ( using genetic, cytological, biochemical, microbiological methods) for the presence of harmful bacteria ( helicobacter pylori), which are most often the cause of non-atrophic gastritis. It is also possible to conduct an immunological blood test for the presence of antibodies ( protective protein molecules circulating in the blood) to Helicobacter pylori.
The main symptom of a stomach ulcer is pain in the upper abdomen. If the ulcer is localized in the cardiac or fundus ( bottom of the stomach) parts of the stomach, then pain occurs immediately after eating. If pain syndrome develops after eating ( after 30 - 60 minutes), and then increases and gradually decreases over 1.5 - 2.5 hours, this indicates the presence of a stomach ulcer in the area of \u200b\u200bhis body.
If abdominal pain occurs 1.5 - 2 hours after eating, then this means that the ulcer is located in the pyloric part of the stomach. Sometimes, with ulcers of the pyloric part of the stomach, pain syndrome can develop a little later - 2.5 to 4 hours after the next meal. The intensity of pain is always individual and depends to a greater extent on the size and location of the ulcer. The pain that appears with a stomach ulcer can radiate ( spread) in different areas of the body ( left shoulder, shoulder blade, spine, lower back, etc.). Painful sensations can often be combined with other symptoms - nausea, vomiting, sour belching, heartburn, loss of appetite, heaviness in the abdomen.
The main instrumental methods that are used in the diagnosis of stomach ulcers are esophagogastroduodenoscopy, intragastric pH-metry, contrast fluoroscopy. With the help of an intragastric pH-meter, the acidity in his stomach is determined in a patient. With contrast fluoroscopy, the patient is given a little bit of a radiopaque contrast agent to drink ( contrast), and then X-rayed his body in order to reveal how this substance passes through the gastrointestinal tract. Getting on the walls of the stomach, the radiopaque substance envelops them and, thereby, shows the shape of the stomach. In the presence of an ulcer in the stomach wall, the contrast agent is retained there. In the picture ( radiograph) it looks like a niche.
Esophagogastroduodenoscopy is a much more informative method for diagnosing stomach ulcers than contrast fluoroscopy, since it allows you to visually detect an ulcer, reliably assess its size, the presence of complications, and characterize the state of the gastric mucosa.
For the detection of Helicobacter pylori serving common reason stomach ulcers, with endoscopic examination of the stomach ( esophagogastroduodenoscopy) make a biopsy of his mucous membrane ( that is, they take a piece of it). Further, the pathological material is delivered to the laboratory and tested by various methods ( biochemical, genetic, bacteriological) for the presence of this pathogenic bacteria.
Pyloric stenosis is characterized by the appearance of pain in the abdomen after eating, sour belching, heartburn, nausea, vomiting, and a feeling of fullness in the abdomen. Vomiting often brings relief to the patient. Weight loss, exhaustion, dehydration, headache, dizziness, malaise, and pale skin may also occur.
Esophagogastroduodenoscopy and contrast fluoroscopy help to confirm the diagnosis. The first method allows you to visually discern the obstruction of the pylorus of the stomach, establish the cause ( presence of adhesions, tumors). The second method can also reveal the presence of stenosis of the gastric pylorus, which during the study will be evidenced by a slowdown in the evacuation capacity of the stomach, an increase in its size, a narrowing of its pyloric section and a violation of its peristalsis.
Diagnostics of the causes of belching with bitterness
Belching with bitterness can be combined with other important symptoms such as heartburn, abdominal pain ( at its top), bloating, weight loss, nausea, vomiting, chest pain, a feeling of fullness in the stomach, loss of appetite. All these symptoms are not specific to any disease, but indicate a malfunction of the gastrointestinal system.In addition to asking the patient about his complaints, it is also important to find out from him certain anamnestic data regarding chronic diseases that he suffered in the past ( gastritis, peptic ulcer, cholecystitis, pancreatitis, etc.), operations ( on the stomach, intestines, gallbladder, etc.), bad habits ( smoking, drinking alcohol), lifestyle ( improper diet, physical inactivity), which, to one degree or another, could cause the appearance of belching with bitterness.
Clinical examination of the patient and, in particular, palpation is also important, which allows the doctor to find out the exact area of \u200b\u200bpain. If a disease that causes bitter belching affects the stomach or duodenum ( for example, gastritis, duodenitis, peptic ulcer, etc.), then the pain is usually localized in the upper central part of the abdomen, just below the sternum. Pain can also occur on the right side of the upper abdomen. The presence of such pains and belching bitter most often indicates the pathology of the biliary tract ( gallstone disease, cholecystitis, biliary dyskinesia, tumors of the Vater's nipple, etc.).
With duodenostasis ( stagnation of the contents of the duodenum, as a result of a violation of its patency) using palpation ( and visually) you can detect bloating in the projection of the duodenum, as well as in the stomach.
Duodenogastric and gastroesophageal reflux can be detected using contrast fluoroscopy and esophagogastroduodenoscopy. The same methods, in most cases, allow you to identify the cause ( improper peristalsis, disruption of the lower esophageal sphincter or pylorus, presence of duodenostasis) the appearance of such refluxes. Endoscopic research method ( esophagogastroduodenoscopy) is also necessary to assess the state of the mucous membranes of the esophagus, stomach, intestines and detect pathological changes on them ( ulcers, erosions, tumors, scars, etc.).
In the presence of duodenostasis, esophagogastroduodenoscopy allows the doctor to find out its cause, that is, to detect tumors in the intestinal lumen, foreign bodies, adhesions ( adhesions), helminths, which can simply block the intestinal lumen and disrupt the normal outflow of its contents to the following sections of the small intestine. If the cause of duodenostasis could not be clarified using esophagogastroduodenoscopy, then the patient is prescribed computed tomography and magnetic resonance imaging.
To confirm the presence of duodenogastric and gastroesophageal refluxes, intraesophageal and intragastric pH-metry is used. These studies assess the level of acidity in the esophagus and stomach, respectively. In addition to them, cholecystography and ultrasound examination may be prescribed to assess the condition of the gallbladder and biliary tract.
Diagnostics of the causes of rotten-smelling belching
With atrophic gastritis, patients usually have a decrease in appetite, belching with a foul smell, an unpleasant taste in the mouth, a feeling of heaviness in the stomach after eating, bloating, unstable stools, malaise, headache, dizziness, pale skin, shortness of breath, weakness, decreased ability to work. Pain syndrome is not typical for this disease, but sometimes it still appears in the form of unexpressed, pulling, dull pain in the epigastric region ( abdominal area located below the sternum).During the esophagogastroduodenoscopy, the patient may reveal some pathological changes on the surface of his mucous membrane ( pallor, thinning, smooth relief). Also, this study is necessary to take a section of stomach tissue for further laboratory examinations, which can reveal certain morphological changes characteristic of atrophic gastritis ( death of the glands of the gastric mucosa, a significant decrease in the number of epithelial cells inside it, proliferation of connective tissue, etc.).
In addition, laboratory methods ( biochemical, genetic, bacteriological, etc.), the presence of Helicobacter pylori in the gastric mucosa can be detected. Thus, esophagogastroduodenoscopy makes it possible to assess the state of the gastric mucosa and to suspect its atrophy, and laboratory tests are necessary to confirm the diagnosis and establish the etiological cause of atrophic gastritis.
Intragastric pH-metry is also important in the diagnosis of atrophic gastritis. It allows you to determine the level of acidity in the stomach, assess the severity of the pathology and choose the necessary treatment tactics.
Chronic pancreatitis is accompanied by pain in the abdomen, belching with a foul smell ( sometimes it can be odorless), nausea, vomiting, flatulence ( bloating), loss of appetite, weight, rumbling in the stomach, heartburn, diarrhea ( diarrhea). Pain in this disease can appear in the epigastric region, in the navel or in the left hypochondrium. Sometimes they are shingles. Pain can radiate ( spread) in the left shoulder, scapula, in the region of the heart or in the left corner of the abdomen ( left iliac region). The appearance or aggravation of pain syndrome in chronic pancreatitis is usually associated with food intake ( pain occurs 30 - 60 minutes after eating).
To assess the state of the pancreas, determine its size, shape and detect possible pathological changes ( sclerosis, tumor, cyst, etc.) inside it, the patient is prescribed ultrasound, computed tomography, magnetic resonance imaging. To study the function and condition of the large papilla ( the area where the common duct of the bile and pancreatic tract opens into the duodenum) in the duodenum, esophagogastroduodenoscopy is used.
IN general analysis blood in chronic pancreatitis, leukocytosis can be detected ( an increase in the number of leukocytes in the blood), anemia ( decrease in the number of red blood cells and hemoglobin), increased ESR ( erythrocyte sedimentation rate). In a biochemical blood test for this pathology, an increase in blood glucose levels, an increase in the activity of alpha-amylase, lipase, trypsin, alkaline phosphatase, gamma-glutamyl transpeptidase ( GGTP), a decrease in the amount of total protein, albumins, blood coagulation factors, pancreatic hormones ( somatostatin, insulin, glucagon).
Stool analysis can detect large amounts of undigested or partially digested food. It reveals a high fat content ( steatorrhea), muscle and connective fibers ( creatorrhea) and starch ( amilorrhea).
With stomach cancer, pain in the upper abdomen, nausea, vomiting, heartburn, belching with a rotten smell, decreased appetite, weight loss, a feeling of heaviness and discomfort in the abdomen after eating, unpleasant taste in the mouth, headache, dizziness, decreased ability to work , unstable stools, bloating, weakness, fever, swallowing problems, jaundice, enlargement of the liver and spleen in size, swelling in the legs and arms, pale skin.
Stomach cancer is diagnosed based on the results of radiation, endoscopic and laboratory research methods. The main radiation methods used in the diagnosis of stomach cancer are computed tomography, magnetic resonance imaging, contrast fluoroscopy, and ultrasound.
Esophagogastroduodenoscopy is important in such patients. This method allows not only to detect a volumetric formation in the stomach cavity, as is done by radiation methods of research, but also to conduct a biopsy ( take a piece) tumor tissue. Biopsy ( a piece of tumor tissue taken from a biopsy) is then delivered to the laboratory for cytological examination, which can confirm the presence of a tumor and establish its type.
Treating the causes of belching
 All pathologies that cause belching, in the vast majority of cases, are treated with medication. In some cases ( for example, with aerophagia) doctors do not prescribe them at all. Surgery it is used very rarely and only if the patient has a severe disease of the gastrointestinal system ( swelling of the stomach, intestines, hiatal hernia, etc.). Since there are several types of belching ( sour belching, bitter belching, etc.), then for convenience all treatment of the causes of belching can be divided into categories or sections.
All pathologies that cause belching, in the vast majority of cases, are treated with medication. In some cases ( for example, with aerophagia) doctors do not prescribe them at all. Surgery it is used very rarely and only if the patient has a severe disease of the gastrointestinal system ( swelling of the stomach, intestines, hiatal hernia, etc.). Since there are several types of belching ( sour belching, bitter belching, etc.), then for convenience all treatment of the causes of belching can be divided into categories or sections. The following sections of the treatment of the causes of belching are distinguished:
- treatment of the causes of belching with air;
- treating the causes of sour belching and heartburn;
- treatment of the causes of belching with bitterness;
- treating the causes of foul-smelling belching.
Treatment of the causes of belching with air
Specific drug treatment aerophagia does not. To get rid of belching with air, the patient should adhere to certain rules for eating. It should be consumed in small portions 4-6 times a day. In this case, you need to eat slowly. When you eat, don't talk. From the diet, you need to exclude carbonated drinks, foods containing menthol ( mint), coffee, chocolate, heavily seasoned meat products ( sausages, sausages), citrus fruit.It is advisable not to eat dry food. If you have to do this, then you need to drink it with a sufficient amount of liquid. It is recommended to stop smoking, use chewing gum, and drink alcohol. If belching with air in a patient is a symptom of a disease of the gastrointestinal system ( gastritis, stomach ulcer, hiatal hernia, etc.), then it should be cured with appropriate treatment.
Patients with mental and neurological disorders are sometimes prescribed sedatives ( sedatives) and antidepressants. It is important for such patients to control the swallowing act - less often to swallow saliva or phlegm, it is better to spit them out, mentally suppress belching, and also avoid stressful and conflict situations.
Treating causes of acid belching and heartburn
Treatment of the causes of sour belching and heartburn includes conservative and surgical methods. Conservative treatment consists of prescribing a special diet to the patient, which slightly relieves the digestive tract and drugs... Surgical intervention in the treatment of heartburn and sour eructation is rarely used. It can be prescribed, for example, for a hiatal hernia or for stenosis of the pylorus.Gastroesophageal reflux disease
Treatment for gastroesophageal reflux disease consists of general treatments and medication. General treatment measures include the usual recommendations that the doctor gives to the patient before prescribing medication. They relate to adherence to a certain diet ( fractional food intake, food should be consumed at least 3 to 4 hours before bedtime, hot and cold drinks should be avoided), lifestyle ( cessation of smoking, playing sports, using diets that reduce body weight, etc.), exclusion of certain foods from the diet ( coffee, chocolate, tomatoes, citrus fruits, sweets, alcohol, smoked sausages, etc.).
The patient is prohibited from taking drugs that help relax the lower esophageal sphincter ( calcium antagonists, nitrates, antidepressants, etc.), as well as those that have a damaging effect on the mucous membrane of the esophagus ( non-steroidal anti-inflammatory drugs, potassium preparations, etc.).
Antisecretory drugs, antacids and prokinetics are usually prescribed as medical treatment for such patients. The first two groups of funds are prescribed to reduce the production of hydrochloric acid in the stomach ( antisecretory drugs) and lowering acidity in the stomach ( antacids and antisecretory drugs). Prokinetics are prescribed to improve motility in the gastrointestinal system.
Hernia of the esophageal opening of the diaphragm
The choice of treatment method depends on the severity of the pathology. In mild clinical cases, drug treatment is prescribed, which blocks the aggressive effect of gastric juice on the esophageal mucosa. For this, antisecretory drugs and antacids are prescribed. In addition to them, prokinetics are sometimes prescribed, which stimulate peristalsis in the gastrointestinal tract. Drug treatment, in most cases, is compensatory. It cannot completely cure the patient from a hiatal hernia, but only relieves or reduces the intensity of its symptoms.
In some cases, medication may not be effective. Then they resort to surgical intervention, the purpose of which is to restore the normal anatomical relationship of organs in the chest and abdominal cavities. That is, in simple words, the movement of the abdominal organs ( lower esophagus, stomach, intestines) in place and strengthening the esophageal opening of the diaphragm to prevent recurrence ( repetitions) hernia.
Scleroderma
The main groups of drugs used in the treatment of scleroderma are immunosuppressants ( suppress immune responses) and glucocorticoids ( steroidal anti-inflammatory drugs). As an additional treatment, the doctor may prescribe antisecretory drugs ( reduce the production of hydrochloric acid in the stomach), antacids ( neutralize hydrochloric acid) and prokinetics ( stimulate motility in the gastrointestinal system).
Additional treatment is symptomatic and aimed at eliminating the negative effect of gastric contents on the mucous membrane of the esophagus in gastroesophageal ( gastroesophageal) reflux, appearing with scleroderma and causing sour belching and heartburn.
Non-atrophic gastritis
With non-atrophic gastritis, fractional nutrition is prescribed, products that irritate the gastric mucosa are excluded from the diet ( salty, peppery, fatty, marinades, smoked dishes, etc.). The patient's food should be prepared by cooking, steaming, or baking. It is not recommended to eat fried foods, canned food, various sauces ( mayonnaise, ketchup, mustard, etc.), alcohol, coffee, pastry products, soda water, some dairy products ( kefir, milk, sour cream).
In addition to the diet, patients with such gastritis are prescribed drug treatment. It consists of antisecretory drugs that suppress the secretion of gastric juice in the stomach and antacids ( neutralize hydrochloric acid and pepsin, and also protect the gastric mucosa). Gastroprotective agents ( agents that envelop and protect the gastric mucosa) and antibiotics. Antibiotics are prescribed in the event that Helicobacter pylori has been identified in the stomach using laboratory tests.
Stomach ulcer
With a stomach ulcer, a diet is prescribed that excludes the use of food ( salted, peppery, smoked, fried, canned food, etc.), irritating the intestinal mucosa and causing increased secretion of gastric juice. All food is recommended to be steamed or boiled. Since stomach ulcer in 90 - 95% of cases is associated with H. pylori infection, the basis of treatment this disease makes up the appointment of antibiotics. To reduce the formation of gastric juice in the stomach, antisecretory drugs are prescribed. To increase the protective properties of the gastric mucosa, gastroprotectors and antacids are prescribed.
Pyloric stenosis
With stenosis of the gastric pylorus, surgical intervention is necessary to eliminate its cause and restore normal patency between the two parts of the gastrointestinal system - the stomach and small intestine.
Treatment of the causes of belching with bitterness
Various groups of drugs are used to treat the causes of bitter belching. The choice of each group depends on the very reason. However, in most of these cases, antacids are prescribed ( neutralize hydrochloric acid), antisecretory drugs ( reduce the formation of hydrochloric acid in the stomach), bile acid inhibitors ( bind free bile), prokinetics ( improve the motility of the stomach and intestines). If the belching of bitterness is caused by dyskinesia of the bile ducts, then in such cases, cholagogues and antispasmodics are prescribed. These drugs improve the flow of bile into the duodenum from the biliary tract.Atrophic gastritis
If atrophic gastritis was caused by Helicobacter pylori, then various antibiotics are prescribed. To date, no etiotropic treatment has been developed for autoimmune atrophic gastritis. Also, with atrophic gastritis, anti-inflammatory drugs of plant origin are prescribed ( infusion of St. John's wort, plantain, chamomile, etc.), vitamins and replacement therapy, that is, drugs that include components of gastric juice.
Chronic pancreatitis
In chronic pancreatitis, the patient can be prescribed a large variety of drugs, due to the fact that with this pathology there are many disorders both in the gastrointestinal system and beyond.
For the treatment of chronic pancreatitis, the following groups of drugs are used:
- Analgesics. Analgesics or pain relievers ( baralgin, analgin, promedol, etc.) is prescribed to eliminate the pain syndrome that occurs in chronic pancreatitis.
- Antienzyme drugs.Since in chronic pancreatitis, the pancreas's own enzymes damage its tissue, their inhibitors are prescribed ( antienzyme drugs) - kontrikal, aprotinin, gordox.
- Antisecretory drugs.One of the important stimulants of pancreatic secretion is gastric juice, therefore, for the successful treatment of chronic pancreatitis, it is necessary to reduce its secretion in the stomach, for which, in fact, antisecretory drugs are prescribed ( lansoprazole, omeprazole, etc.).
- Pancreatic enzymes.Since in chronic pancreatitis there is exocrine pancreatic insufficiency, substitution therapy is prescribed in the form of drugs (
Why is belching accompanied by a heaviness in the abdomen?
 In some cases, belching can be combined with a heaviness in the abdomen. This is usually observed in diseases ( stomach cancer, atrophic gastritis, hiatal hernia, chronic pancreatitis, etc.), accompanied by a violation of the movement of food through the gastrointestinal system. With these diseases, food stagnates in the stomach and intestines, as a result of which intracavitary pressure increases in these organs ( that is, the pressure inside the organ).
In some cases, belching can be combined with a heaviness in the abdomen. This is usually observed in diseases ( stomach cancer, atrophic gastritis, hiatal hernia, chronic pancreatitis, etc.), accompanied by a violation of the movement of food through the gastrointestinal system. With these diseases, food stagnates in the stomach and intestines, as a result of which intracavitary pressure increases in these organs ( that is, the pressure inside the organ).High pressure acts on the nerve endings that innervate the lining of the stomach and intestines, which gives the patient a feeling of heaviness in the abdomen. These two symptoms can also occur if a person does not have any pathology in the gastrointestinal system. This is often the case with a combination of overeating and aerophagia ( that is, swallowing excess air at the time of eating), as well as when drinking a lot of carbonated water.
Why does the upper abdomen hurt when belching?
 Pain in the upper abdomen during belching most often indicates the presence of a pathology in the patient's gastrointestinal system. If this pathology of the stomach, then the pain in the upper abdomen, in most cases, is caused by damage and inflammation of its mucous membrane, which is often found with a tumor or stomach ulcer, gastritis ( inflammation of the stomach lining). If this is a pathology of the duodenum ( for example, a tumor, intestinal ulcer, duodenitis, etc.), then pain in such cases, they are provoked by the defeat of its mucous membrane and stretching of its wall.
Pain in the upper abdomen during belching most often indicates the presence of a pathology in the patient's gastrointestinal system. If this pathology of the stomach, then the pain in the upper abdomen, in most cases, is caused by damage and inflammation of its mucous membrane, which is often found with a tumor or stomach ulcer, gastritis ( inflammation of the stomach lining). If this is a pathology of the duodenum ( for example, a tumor, intestinal ulcer, duodenitis, etc.), then pain in such cases, they are provoked by the defeat of its mucous membrane and stretching of its wall. With gastroesophageal reflux disease, hiatal hernia and scleroderma, damage to the esophageal mucosa occurs as a result of the reflux of gastric contents into the esophagus, which has an aggressive effect on it. Such a lesion is often accompanied by pain and burning in the upper abdomen and behind the breastbone.
Why does belching occur during pregnancy, what should I do?
 The appearance of belching during pregnancy is a completely normal reaction from the organs of the gastrointestinal tract. It occurs due to an increase in intra-abdominal pressure due to an increase in the size of the uterus. During the growth of the fetus, the uterus of the pregnant woman begins to squeeze the intestines, which leads to a slowdown in the movement of feces along it, the formation of duodenostasis ( stagnation in the duodenum) and violation of the evacuation of food from the stomach into the intestines. All this causes the formation of an excessive amount of gases under the influence of the microflora in the gastrointestinal system.
The appearance of belching during pregnancy is a completely normal reaction from the organs of the gastrointestinal tract. It occurs due to an increase in intra-abdominal pressure due to an increase in the size of the uterus. During the growth of the fetus, the uterus of the pregnant woman begins to squeeze the intestines, which leads to a slowdown in the movement of feces along it, the formation of duodenostasis ( stagnation in the duodenum) and violation of the evacuation of food from the stomach into the intestines. All this causes the formation of an excessive amount of gases under the influence of the microflora in the gastrointestinal system. It should be noted that gas formation is also promoted by the disorder of the motility of the digestive tract, which appears as a result of hormonal changes in the body of a pregnant woman. Belching in such cases is not constant, is not combined with other symptoms ( abdominal pain, heartburn, vomiting, etc.) and often occurs with errors in power supply.
If a pregnant woman's belching occurs periodically and at the same time it is accompanied by heartburn, dysphagia ( swallowing disorder), shortness of breath, cough, hoarseness, feeling of a lump in the throat, nausea, vomiting, hiccups, pain in the heart, throat, chest, abdomen, fever or bloating, then you need to go for a consultation with the doctor supervising this patient. Self-medication in such cases is dangerous to deal with, since, firstly, it is not known which pathology could cause these symptoms and, secondly, many drugs have certain contraindications and not all of them can be used during pregnancy.
Why does belching and bloating occur, what should I do?
 Belching is often associated with bloating. This symptom usually indicates the presence of excess gas inside the stomach or intestines. Gas formation in these organs occurs either due to digestion ( that is, normal), or as a result of the appearance in them of pathological processes of putrefaction or fermentation, which are often found in diseases of the organs of the gastrointestinal system ( pancreas, liver, biliary tract, stomach, small intestine).
Belching is often associated with bloating. This symptom usually indicates the presence of excess gas inside the stomach or intestines. Gas formation in these organs occurs either due to digestion ( that is, normal), or as a result of the appearance in them of pathological processes of putrefaction or fermentation, which are often found in diseases of the organs of the gastrointestinal system ( pancreas, liver, biliary tract, stomach, small intestine).
Bloating and belching can normally occur with overeating, drinking significant amounts of soda, accidentally swallowing air while smoking, chewing gum, talking while eating, and eating quickly. In such cases, these two symptoms are not permanent and, as a rule, are clearly associated with one of the listed factors ( smoking, drinking soda, etc.). Elimination of this factor ( for example, eating on time, eating in silence, etc.) usually prevents new episodes of belching and bloating.If you experience constant belching and bloating, it is advisable to immediately apply for medical help to a gastroenterologist. This must be done in order to reliably find out the exact cause of these two symptoms and choose the right treatment, since not all diseases of the gastrointestinal system are treated equally.
Why is there nausea when belching?
 Nausea is a rather unpleasant and painless sensation that is often a harbinger of vomiting. This symptom also serves as an indispensable sign of a disorder in the function of the gastrointestinal system. The occurrence of nausea, with the simultaneous presence of belching in the patient, is usually associated with impaired gastric motility and a decrease in the production and secretion of gastric juice in it. It is believed that the feeling of nausea in these patients is caused by antiperistaltic ( reverse peristalsis) movements of the stomach.
Nausea is a rather unpleasant and painless sensation that is often a harbinger of vomiting. This symptom also serves as an indispensable sign of a disorder in the function of the gastrointestinal system. The occurrence of nausea, with the simultaneous presence of belching in the patient, is usually associated with impaired gastric motility and a decrease in the production and secretion of gastric juice in it. It is believed that the feeling of nausea in these patients is caused by antiperistaltic ( reverse peristalsis) movements of the stomach. What pathologies cause a lump in the throat and belching?
 A lump in the head and belching are most common with hiatal hernia, systemic scleroderma, and gastroesophageal reflux disease. With a hernia of the esophageal opening of the diaphragm and gastroesophageal reflux disease, a lump in the throat appears due to the fact that with these pathologies, reflux esophagitis is often observed ( inflammation of the lining of the esophagus resulting from gastroesophageal reflux) and frequent reflux of food from the stomach into the esophagus, and sometimes into the throat.
A lump in the head and belching are most common with hiatal hernia, systemic scleroderma, and gastroesophageal reflux disease. With a hernia of the esophageal opening of the diaphragm and gastroesophageal reflux disease, a lump in the throat appears due to the fact that with these pathologies, reflux esophagitis is often observed ( inflammation of the lining of the esophagus resulting from gastroesophageal reflux) and frequent reflux of food from the stomach into the esophagus, and sometimes into the throat. With systemic scleroderma, the muscle and mucous layers of the esophagus are damaged, as a result of which its motility and mucus secretion are impaired, which makes it difficult to move swallowed food. It sometimes gets stuck in the throat, which gives these patients a feeling of a lump in it.
Why is there pain in the right hypochondrium and belching?
 Pain in the right hypochondrium and belching are usually signs of hepatobiliary pathology ( hepatobiliary) systems ( cholecystitis, cholelithiasis, biliary dyskinesia, etc.). The appearance of pain in the right hypochondrium in such cases is caused by inflammatory and destructive processes in the tissues, which are noted in these pathologies ( for example, pain in cholecystitis is caused by inflammation of the gallbladder mucosa).
Pain in the right hypochondrium and belching are usually signs of hepatobiliary pathology ( hepatobiliary) systems ( cholecystitis, cholelithiasis, biliary dyskinesia, etc.). The appearance of pain in the right hypochondrium in such cases is caused by inflammatory and destructive processes in the tissues, which are noted in these pathologies ( for example, pain in cholecystitis is caused by inflammation of the gallbladder mucosa).In diseases of the liver and biliary tract, there is also a violation of the delivery of bile to the duodenum. This is due either to obstruction of the biliary tract, or to the fact that little bile is produced in liver cells. Since bile plays an important role in digestion ( it emulsifies fats, stimulates intestinal peristalsis, activates some digestive enzymes, has bactericidal properties, etc.), then its absence does not go away for the body is not noticeable.
In the intestine, digestion processes slow down, harmful microbes begin to multiply. In the process of their growth, they begin to produce a large amount of gas, which is partially removed through the stomach and partially passed on to other parts of the intestine. Gas that enters the stomach can at some point enter the esophagus and further into oral cavity... The ingress of gases from the esophagus into the oral cavity is accompanied by belching.
Why is there a belching and burning sensation in the throat and / or esophagus?
 Belching and burning in the throat and / or esophagus are associated with gastroesophageal ( gastroesophageal) refluxes ( back-throwing food), which can be observed in certain pathologies of the gastrointestinal system ( gastroesophageal reflux disease, systemic scleroderma, non-atrophic gastritis, pyloric stenosis, hiatal hernia, stomach ulcer, etc.).
Belching and burning in the throat and / or esophagus are associated with gastroesophageal ( gastroesophageal) refluxes ( back-throwing food), which can be observed in certain pathologies of the gastrointestinal system ( gastroesophageal reflux disease, systemic scleroderma, non-atrophic gastritis, pyloric stenosis, hiatal hernia, stomach ulcer, etc.).With these refluxes, the contents of the stomach pass into the esophagus. If they ( refluxes) appear in the patient periodically, the contents of the stomach cause damage to the mucous membrane ( and also contained therein nerve endings ) of the esophagus and causes inflammation in it. With such inflammation, only a burning sensation in the chest is observed ( esophagus).
Sometimes gastroesophageal refluxes can be quite high and reach the pharynx. In such cases, burning is already observed not only in the esophagus ( sternum), but also in the throat ( due to inflammation of its mucous membrane and damage to the nerves that innervate it). The penetration of gases from the stomach into the esophagus, and then into the oral cavity during gastroesophageal reflux, explains the mechanism of belching in these patients.
In what diseases can belching and diarrhea occur?
 Belching and diarrhea ( diarrhea) quite often occur in diseases accompanied by impaired secretion of digestive substances ( enzymes, hydrochloric acid, bile, etc.) and slowing down the movement of food through the digestive system. This is observed in atrophic gastritis, chronic pancreatitis, stomach cancer, biliary dyskinesia, cholecystitis, duodenitis ( inflammation of the duodenal mucosa).
Belching and diarrhea ( diarrhea) quite often occur in diseases accompanied by impaired secretion of digestive substances ( enzymes, hydrochloric acid, bile, etc.) and slowing down the movement of food through the digestive system. This is observed in atrophic gastritis, chronic pancreatitis, stomach cancer, biliary dyskinesia, cholecystitis, duodenitis ( inflammation of the duodenal mucosa). With these diseases, dysbiosis occurs, in which harmful microbes begin to multiply in the gastrointestinal system. In the process of their vital activity, many toxins are formed in the stomach and intestines, which adversely affect the mucous membrane of the latter, as a result of which it becomes inflamed and begins to intensively secrete water into its lumen. Therefore, these patients develop diarrhea. With dysbiosis, a large number of gases are also formed. One of the mechanisms for their removal from the gastrointestinal tract is their release into the oral cavity ( here they penetrate through the esophagus from the stomach), which is accompanied by belching.
Absolutely different symptoms in some cases may indicate the same disease. For example, belching with air and a lump in the throat - the causes of one disease, or does their appearance indicate a violation of various body functions and do not depend on each other?
It seems to many that belching signals a violation of the digestive tract, however, this opinion may be erroneous and the reason lies in a completely different pathology. In our article, we will consider what causes the appearance of these symptoms and whether it is possible to recognize the ailment based on these symptoms.
Symptoms such as a lump in the throat and belching with air can appear independently of each other, however, their joint manifestation indicates common cause occurrence. Let us consider in more detail the causes of the appearance of these symptoms together and separately.
What does the separate appearance of symptoms indicate?
As a result of medical research, scientists have come to the conclusion that such a manifestation as belching gets stuck in the throat, forming a strange sensation of air in the throat, indicates muscle spasm. The main reason lies in the natural process of swallowing food, when a lot of air enters the throat with food, thereby causing discomfort. However, if, heartburn, belching with air is a reason to immediately consult a doctor.
The sensation of a lump in the throat arises due to some pathological processes:
- spasm of the muscles of the esophagus;
- inflammatory process mucous membrane for a long time;
- neoplasms in the pharynx;
- the presence of a foreign agent in the throat.
With such pathologies, usually occurs strong pain in the throat when belching, the feeling of the presence of air increases.
Belching in a separate manifestation indicates a large amount of air swallowed with food. Or it is increased gas formation in the stomach, which causes intragastric pressure and contraction of the muscles of the digestive system, while the cardinal pulp relaxes.
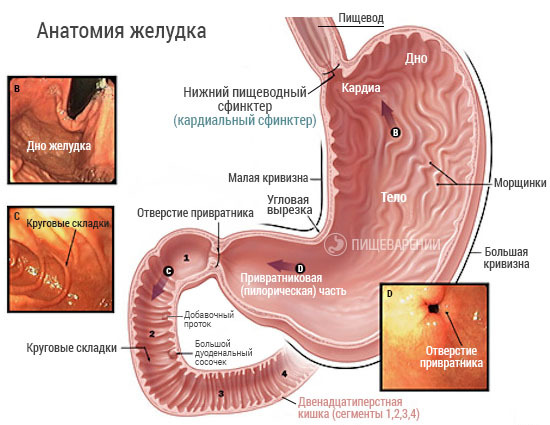
For a visual representation of the work of the digestive system, the photo below shows the anatomy of the stomach:
Interesting fact. Most often, the female population of the planet is faced with symptoms such as belching and a lump in the throat. Cases of manifestation of pronounced carcinophobia and fear of detecting cancer are not uncommon. A lump in the throat makes them think about possible neoplastic neoplasms in the pharynx.
Belching, accompanied by a feeling of a lump in the throat, is divided into two types:
- belching with air;
- belching with an unpleasant odor.
Belching with air does not cause any particular inconvenience to the patient, but with an unpleasant smell it causes discomfort, both to the patient himself and to those around him. It indicates stagnation of food in the stomach. When bile enters, an eructation with a bitter taste erupts, with low acidity, sour belching is present.
Important. Belching with a putrid odor, which often resembles the smell of a rotten egg, indicates liver dysfunction. With these symptoms, you should undergo an examination, pass the necessary tests and start treatment in a timely manner.
When a lump in the throat and belching are the result of the same disease?
When a lump in the throat and belching appears together, the causes can be different. It is observed both in absolutely healthy people and in people suffering from chronic diseases Gastrointestinal tract. Pregnant women often experience symptoms, mostly after eating.
In the table below, we will consider in detail the diseases characterized by the joint manifestation of symptoms:
| Disease | Associated symptoms |
| Inflammation of the lining of the esophagus (esophagitis) | After eating, there is a burning sensation in the esophagus. Constant or paroxysmal pain in the chest area that radiates to the lower jaw, shoulders or the area between the shoulder blades. A lump appears in the throat after eating, belching with air. The movement of the lump along the esophagus is felt, which also indicates a violation of the functions of muscle tissue. In some cases, regurgitation is observed (return of food from the stomach to the mouth). |
| Gastroesophageal reflux disease (GERD) | It is characterized by an inflammatory process of the esophageal mucosa and dysfunction of the lower esophageal sphincter. The esophageal sphincter is located in the lower third of the esophagus, it is a round muscle responsible for delimiting the two sections (stomach and esophagus). Prevents the return of food. It is also characterized by inflammation of the gastric mucosa, which leads to increased secretion of gastric juice, which causes heartburn, nausea, lump in the throat, belching. There may also be pain behind the sternum, radiating to the left shoulder blade and shoulder. In rare cases, vomiting, coughing, shortness of breath, general malaise, insomnia appear. |
| Neurosis | Neurosis can also be attributed to the causes of the onset of symptoms. The reaction of the nervous system to various stressful situations rarely passes without visible consequences. In addition to the depression, a lump in the throat and constant belching appear. After an experienced neurosis, a person reacts sharply to events happening around him, therefore, while eating, he nervously swallows food with a large amount of air. As a result, belching appears, and a lump in the throat indicates a violation of the nervous system, but not the work of the esophagus. |

With diseases of GERD and esophagitis, it will not be enough to conduct clinical analyzes, they require a more serious approach, the result of which will be an in-depth examination of the body. First of all, such patients are prescribed FGDS (fibrogastroduodenoscopy) of the upper part of the esophagus, stomach and duodenum.

The appearance of a lump in the throat and belching may indicate the simultaneous course of various ailments.
Two pathologies that do not depend on each other can appear simultaneously, for example:
- Thyroid dysfunction and gastritis. Impaired thyroid function is manifested by a feeling of a lump in the throat, and gastritis is characterized by the appearance of belching.
- The presence of the patient. As a result of which there is a lump in the throat, and belching is manifested due to improper nutrition.
Council. If signs appear, you should contact a gastroenterologist, in this case, self-medication is categorically not recommended, since you can lead to the development of more severe pathologies with your own hands, which can only be cured by surgery.
Why does it appear in healthy people?
Basically, there is an eructation and a lump in the throat after eating, namely, its misuse.
In a healthy person, the onset of symptoms is characterized by:
- fast food intake;
- irregular reception;
- physical activity immediately after eating;
- overeating or malnutrition;
- chewing gum;
- the use of carbonated drinks and preservatives in large quantities.

Council. If symptoms are observed constantly after each meal, this is a signal to sound the alarm and contact a gastroenterologist. It is highly likely that the reason lies in a dysfunction of the digestive system.
Treatment
To get rid of coma and belching, you should determine the cause of their appearance and deal with it.
For each disease, treatment is carried out accordingly:
- Symptoms are caused by stress... It is necessary to resort to relaxation options (relaxing bath with aromatic oils, yoga, light music, outdoor recreation away from the bustle of the city). A severe form of mental disorder requires specialist advice and the use of sedative medications that are prescribed only by the attending physician.
- Gastrointestinal diseases... An in-depth examination of the body and consultation with a gastroenterologist are required. The instruction for drug treatment is prescribed only by the attending physician in accordance with the results of the examination. In addition to drug therapy, physical exercise is recommended to restore the work of the lower sphincter, as well as diet.
- In case of dysfunction of the thyroid gland. The examination is carried out by an endocrinologist, according to the results of blood tests for hormones, an ultrasound examination, he prescribes the appropriate treatment. With a slight increase in the volume of the thyroid gland, they resort to taking iodine-containing preparations and adhere to a diet appropriate for this disease. The neglected form of the disease requires surgical intervention.
Attention. Due to the fact that the cause of the appearance of belching and a lump in the throat is far from always harmless, the appointment of drug therapy is set only by the attending physician. Due to the fact that the price for some drugs may not be affordable for many, one or another drug can be replaced only on the advice of a doctor.
Whatever the etiology of constant belching and a lump in the throat, self-medication in this case is strictly prohibited. The maximum that the patient can do is to lead a correct lifestyle, give up bad habits, observe proper nutrition, rest, etc.
The air emitted during belching leaves the stomach, which contains about 1.5 liters. This allows you to maintain a certain level of pressure in an organ isolated from the external environment. Excess air leaves the intestine, is absorbed by its mucous membrane, but most often it enters the esophagus, and from there into the mouth. All this happens from time to time and is considered the norm. It is quite another matter if this happens day after day. In such cases, only a specialist can find out the reasons for constant belching with air and offer a solution to the problem.
Etiology of the problem
You can understand the reasons for regular belching of air in adults by considering how the digestive system actually works. Moving along the esophagus, food ends up in the stomach. If there is a lot of it and it occupies the entire volume of the stomach, then the air simply has nowhere to go, and it leaves the overflowing stomach through the mouth in the form of belching. This process is evidence of normal gastrointestinal motility.
Therefore, there is no pathology in the fact that after a hearty dinner, air is released from the mouth, and odorless.
- Belching can be provoked by physical exertion, accompanied by a sharp displacement of food inside the stomach, due to which part of the air is ejected into the external environment.
- Tight clothing and tight belts can also cause the phenomenon. This interferes with the expansion of the stomach during meals and forces air to escape to make room for its contents. The phenomenon is common in obese people and occurs a few minutes after eating.
- Frequent belching occurs during pregnancy, especially in the third trimester. The condition is not pathological and is explained by the fact that the enlarged uterus begins to press on the stomach and displaces air from it.
- Sometimes belching of air from the stomach can be triggered by inappropriate eating habits or inappropriate diet. Eating food on the go without chewing it thoroughly, talking while eating cause aerophagia, that is, swallowing air. This also occurs after frequent inhalation, deep breathing, smoking, chewing gum, and wearing uncomfortable dentures. This increases the volume of air in the lumen of the stomach and returns the excess part back to the external environment.
The above cases of belching are rare. But with frequent regurgitation, it is important to find out the reason, which can be difficult to do.
Foods as a cause of belching with air

Carbonated drinks containing dissolved carbon dioxide have such properties.
Eliminating these foods from the diet relieves the unpleasant symptom.
Pain in the epigastric region and belching with air are often combined symptoms.
In addition to them, they may be concerned about:
- nausea;
- heartburn;
- bloating.
If you tortured belching with air, then this may be due to:
- malignant neoplasms;
- GERD (gastroesophageal reflux disease);
- weakness of the sphincter located on the border between the stomach and the duodenum;
- hernia of the opening of the diaphragm;
- cholecystitis;
- duodenitis and gastroduodenitis;
- pancreatitis;
- peptic ulcer;
- atrophic or non-atrophic gastritis.
About the taste and smell of belching

The discharge of gastric juice is the cause of the sour taste of belching.
This happens with diagnoses:
- stomach ulcer;
- reflux disease.
The bitterness in belching is caused by bile, which is known to be produced by the largest gland, the liver. Through special ducts, bile enters the duodenum. A bitter eructation indicates that the emitted air has passed the way from the duodenum through the stomach and into the esophagus.
This symptom accompanies the following diseases:
- dyskinesia;
- cholecystitis;
- pancreatitis.
The most unpleasant symptoms include belching with the smell of rotten eggs.
This is how hydrogen sulfide smells - a gas that is produced by bacteria. This is evidence of low acidity of gastric juice, since microorganisms are unable to survive in conditions of high concentration of caustic hydrochloric acid. This circumstance is accompanied by atrophic gastritis - a pathology in which the gastric mucosa degrades, which leads to a decrease in the number of glands secreting gastric juice. Scleroderma of the esophageal mucosa can also cause air to escape.
Constant belching, especially not associated with food intake, that is, occurring on an empty stomach, is already a cause for concern. Especially if the air smells like rotten eggs, and the discarded contents have a bitter or sour taste. Regular repetitions of this phenomenon are most likely evidence of a developing digestive pathology.
GERD
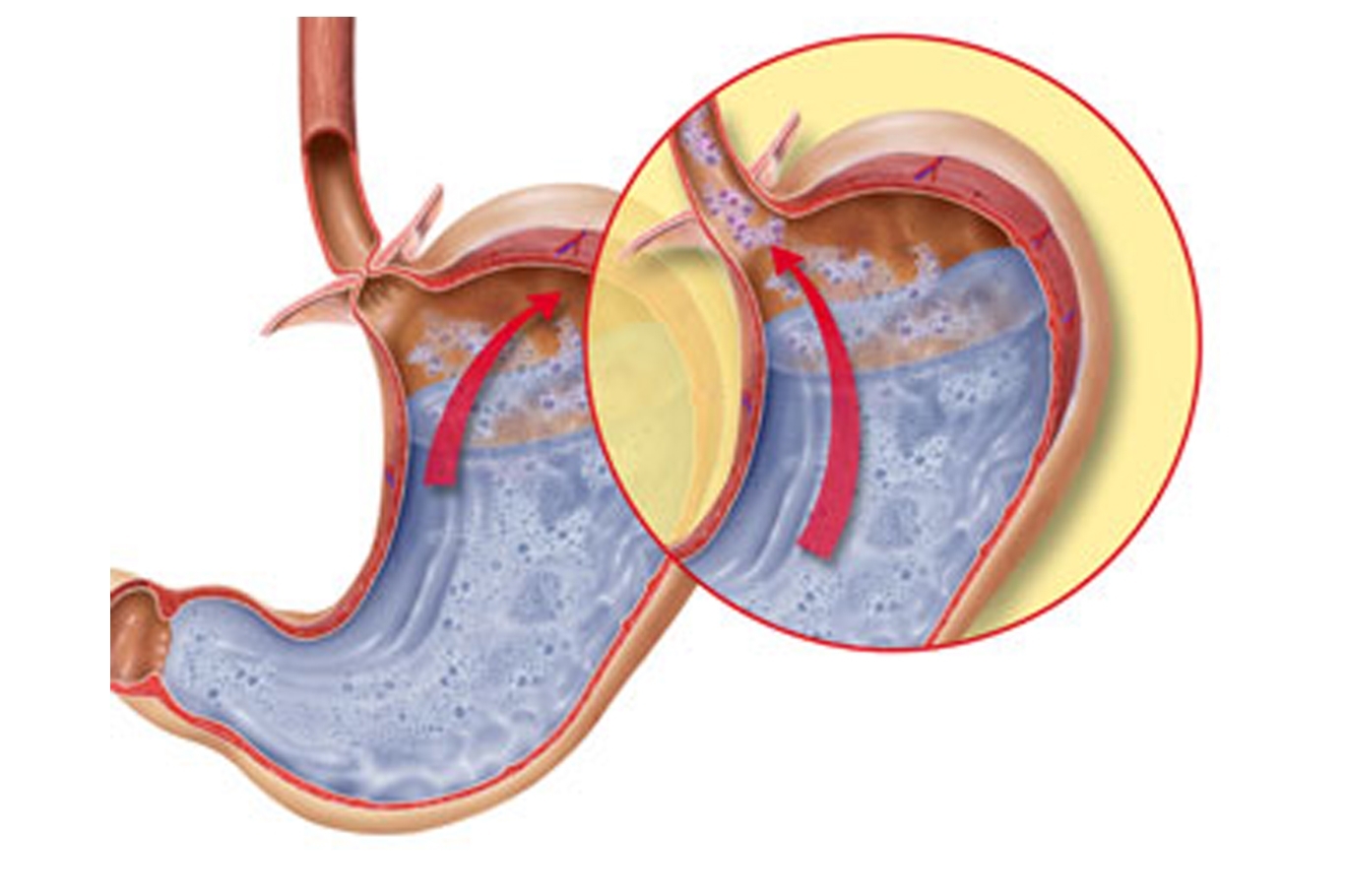
Gastroesophageal reflux disease is the most common cause of regurgitation. This is caused by incomplete closure of the sphincter separating the esophagus from the stomach. This causes frequent reflux of food from the stomach into the pharynx, which causes heartburn or severe burning of the esophageal mucosa, which is hypersensitive to the high acidity of gastric juice. Often occurs when the body is tilted or lying for a long time.
In addition to belching, GERD is accompanied by:
- trouble swallowing;
- pharyngitis;
- arrhythmia;
- dyspnea;
- bloating;
- cough;
- fast saturation;
- soreness in the left side of the chest.
GERD can result from:
- smoking;
- eating while lying down;
- hypodynamia;
- overeating;
- taking some medications;
- drinking coffee, chocolate and citrus fruits.
The disease can lead to an ulcer or erosion of the esophagus.
Gastritis
Belching with air often worries those who suffer from gastritis - an inflammatory process that has invaded the mucous membrane of the gastric wall.
Distinguish gastritis:
- non-atrophic, in which secretory functions are preserved;
- atrophic, when the inflammatory process reduces the secretion of gastric juice.
The atrophic form of the disease is accompanied by: fast saturation, loss of appetite, unpleasant smell of belching air. Pathology leads to vitamin B12 deficiency and anemia, which can be recognized by dry and pale skin, brittle nails and general weakness.
The provocateurs of non-atrophic gastritis are the bacteria Helicobacter pylori.
The disease is accompanied by the frequent discharge of half-digested food from the stomach into the esophagus and sour belching. This form of gastritis is facilitated by taking certain medications and improperly organized meals.
Peptic ulcer
Frequent belching of air is one of the symptoms of stomach ulcers. The disease leads to degradation of the gastric wall, including the exposure of a layer of muscle tissue.
Malignant neoplasms in the stomach area resemble atrophic gastritis in symptoms, but differ in a more severe and progressive course. The patient does not want to eat, especially animal proteins, loses weight, suffers from anemia, heaviness in the stomach, fast satiety.
Diseases of the esophagus
A group of pathologies in which the esophagus can narrow at its bottom or expand at the top.
Problems with the esophagus can be judged by the following signs:
- losing weight;
- belching;
- a lump in the throat;
- difficulty swallowing;
- heartburn.
Eating can be difficult due to irreversible changes and inflammation of the esophagus.
Belching with air can be caused by scleroderma of the esophagus, in which its mucosa ulcerates. Scleroderma can result from burns and injury. Genetic predisposition is also of no small importance in its occurrence.
Duodenal Gastric Reflux
A syndrome in which the bitter contents of the duodenum with bile and pancreatic enzymes end up in the pharynx.
Belching supragastric
An arbitrary form of belching that a person can intentionally cause. With such complaints, you have to resort to the help of a psychotherapist.
The diaphragm is a muscular wall located between the body cavities: chest and abdominal. The lower part of the esophagus passes through a special opening in the diaphragm. If the latter is damaged, problems arise with the movement of food. For example, with a hernia of the diaphragm, belching of air occurs, which is accompanied by pain, heartburn, bitterness in the mouth and heart rhythm disturbances.
Dysbacteriosis
A condition that develops when taking antibiotics and an infection of the intestine. It is accompanied by belching with a rotten smell, lack of appetite, nausea and heartburn.
Pancreatitis
This is the name of the inflammation of the pancreas. The disease is accompanied by nausea and vomiting, alternating constipation and diarrhea, pain in the abdomen and the release of air into the esophagus.
Belching with stomach pain

A combination of unpleasant symptoms occurs for the following reasons:
- Sleep after eating, during which food is not digested properly. This condition can be a harbinger of gastroenterocolitis.
- Belching after water can occur after drinking cold drinks, which interfere with lipid absorption and normal fermentation.
- Bathing after meals leads to an increase in blood flow in the extremities and its slowdown in the stomach and intestines, which weakens digestion and is accompanied by sharp pain in the abdomen and belching.
- Tea. Tea enzymes change the structure of proteins and thus complicate their digestion.
- Violent and persistent belching of air after a meal can be triggered by fresh fruit for dessert, which impairs absorption because organic acids from their composition react with minerals from the main food.
- Smoking. After eating a cigarette causes air and smoke to be swallowed, followed by belching and stomach pain.
Diagnostics
Belching with air, and constantly, deserves the most close attention... A gastroenterologist will help to find out the reason for the regular occurrence.
You can determine the causes and competent treatment of belching with air after a series of studies:
- A blood test will show the presence of inflammation and anemia.
- Stool examination will reveal the source of the infection and the insufficient functioning of the digestive system.
- Anamnesis data, namely, information regarding the diet, diet and day of illness. On a visual examination, the doctor identifies areas where soreness and bloating are present.

If necessary, the doctor prescribes instrumental diagnostic methods:
- radiography with contrast;
- endoscopy with visual examination of the alimentary canal;
- tissue biopsy;
- pH-metry to find out the acidity level of the parts of the gastrointestinal tract;
The above diseases are accompanied by the release of air from the stomach. Therefore for correct treatment an accurate diagnosis is required. It is better not to hesitate with this stage, since empty belching occurs both in simple conditions and in serious pathologies, such as cancerous tumors in the digestive organs.
Treatment

Belching with air is not an independent disease and eliminates itself as the underlying pathology is cured. Most often, conservative therapy is used, but surgical treatment is also possible.
- If pathogens have become provocateurs of the disease, then antibacterial therapy is used.
- Increased gastric acidity can be treated with proton pump inhibitors and antacids.
- Enzyme preparations help with pancreatic insufficiency.
- It is possible to treat hypokinetic dyskinesia of the bile ducts and cholecystitis with the help of choleretic drugs.
- Smecta and other sorbents will remove infectious agents from the digestive canal, and antispasmodics will reduce the tone of the muscle layer of the stomach.
Diet

An important part of the complex treatment of pathologies of the gastrointestinal tract is diet therapy. If there is an eructation of air caused by frequent swallowing, elimination of carbonated drinks and beer, milk, ice cream and onions from the diet will help. For diseases of the stomach and intestines, the diet is agreed with the attending physician.
Refusal from chewing gums, which knock the stomach out of normal rhythm due to excessive chewing movements, elimination of alcohol, smoking, and 4-5 meals a day in small portions help to normalize digestion and relieve belching with air.
Simple rules to prevent belching
- Do not talk while eating.
- Chew food, closing your mouth.
- For those suffering from increased salivation, it is better to spit out the saliva rather than swallow it.
- Limit the use of milkshakes and other beverages that are enriched with air bubbles.
- Drinking through a straw increases the volume of air in the stomach, which inevitably leads to belching.
- Pay attention to strengthening the nervous system. If belching torments the air of a neurotic nature, then the person has to work on inhibiting the conditioned reflex, which usually occurs imperceptibly and involuntarily.
- After eating, it is better to take a walk, and not engage in heavy physical labor or just lie down.
Up to 40 years, a person can cope with any amount of food. With age, there is a decrease in enzymatic functions and from excessive gluttony there are problems with the gastrointestinal tract, including excess weight and an unpleasant embarrassment in the form of involuntary regurgitation of air.
